Management report/business plan for reducing CT scan waiting lists.
Executive summary
Imaging technology platforms are essential for healthcare institutions and practices. Computerised (or computed) tomography (CT) represents an important imaging method that numerous physicians refer their patients to, in order to obtain valuable diagnostic data. Hospitals that offer CT scan services to outpatients, can expect a significant financial benefit. On the other hand, there are numerous private radiology services, which represent a significant competition force. This management report will primarily focus on the NHS environment, which employs about 90% of the currently registered radiographers. It is common for CT scanner services to experience excessively long waiting lists, which result in patient’ and doctor dissatisfaction. Data shows that the demand for such services is increasing, while the resources and/or capacity of the current infrastructure remain the same or in decline. UK radiology services are now expected to operate efficiently with lower financial support, combined with increasing cost pressures.
Enhancing CT scan capacity (productivity) and reducing waiting lists can be achieved in several ways. Perhaps the most financially efficient way is to consider solutions that do not involve the purchasing of new equipment. This solution would require more patients to be scanned per hour, longer scanning schedules or (ideally) both solutions combined, which would be expected to have the biggest impact in CT capacity. During the CT operation, technologists undertake the most significant aspect of the service and their professional education can have a significant impact on the CT capacity. Literature shows that additional training of technologists can reduce the error rates, which result in fewer requests for extra scanning by the radiologists and physicians and increase patient throughput. Given the appropriate training, CT technologists could also expedite the recognition of common CT scan patterns that require further imaging; this could result in the technologist performing this extra scan immediately, without the involvement of a radiologist requesting an extra scan. Also, training technologists in efficiently using the IT (PACS) and supporting software can increase the productivity of the department. The financial implications for increasing the CT productivity are significant. Ensuring that technologists’ knowledge and relevant IT expertise are up to date can result in more efficient use of allocated slots, reduced rate of errors and rejections and physician and patient satisfaction. Previous experience in the NHS context has shown that the increase in CT scan productivity is immediate (within 1-2 months), which quickly covers the cost of the technologists’ training. Employers are expected to support CPD for technologists, according to the service provided.
Introduction
CT scanning platforms often experience long waiting lists. This has been well documented in publications originating from within medical institutions and popular newspapers as well. Long waiting lists for CT scans can negatively affect the survival rates of certain groups of patients, such as cancer patients, but it could also act as a serious deterrent for outpatients and push them towards private competitors. NHS senior managers reported that the waiting times are expected to further increase; in comparison to 2010, almost 5 times more patients had to wait for simple diagnostic tests such as a CT scan. The Daily Mail newspaper (2011) published an article exposing the fact that almost 16,000 patients every month are forced to wait more than six weeks for a CT scan. Silvester and Steyn (2008) report that the current situation is either due to increased average demand without an equivalent available capacity or a mismatch of capacity and demand, which is more often the case for CT scanners.
A PEST (political, economic, social and technology factors) analysis can identify several reasons for this extensive dysfunction. Although the current coalition government has promised to support the increasing health costs, Grant et al. (2012) anticipate a significant change in the NHS budget in the coming years; in 2011 alone, the NHS budget was reduced by 20%. Dickson (2009) confirms that the NHS is in the middle of a serious financial crisis. The author believes that unless productivity is significantly increased, the NHS will not meet the current and future demands for health care. Hospitals are already forced to operate under tight budgets, which inevitably results in changes in staffing and resources dedicated to diagnostic services. Given the current financial state, it is obvious that solutions that improve the CT scan capacity with minimal cost will be preferred and studied first. From a social point of view, the consumers (patients) are becoming more accepting towards radiology imaging technologies and show more faith in their diagnostic efficacy. Physicians also seem to request such diagnostic tests a lot more. The combination of these two factors leads inevitably in a significant increase of the demand of CT scanning services and related technologies. On the other hand, this type of imaging platform is a big investment for a public or private institution alike. This fact limits remarkably the number of such platforms that any institution may possess. Ideally, every diagnostic centre would prefer to dedicate a different CT scanner for inpatients and outpatients, but the reality forces the exploration and implementation of other methods of boosting CT scanning productivity. Furthermore, the lack of a unified functional platform for CT scanning platforms can be considered a technological burden to the efficiency and productivity. The variety of different software, hardware and protocols used is unique to each health institution, which requires from the radiologists and technologists to be re-trained every time they switch to a new professional environment and to a certain degree limits their flexibility.
Proposed Service Development
Encouraging continuous professional development (CPD) of the technologists working in the CT scan services may be a simple but powerful way to boost productivity. CT technologists are required to perform a variety of specialised tasks associated with the operation of CT scanners and related equipment in accordance with prescribed radiation safety procedures. They must also be able to understand and accurately interpret the physician’s scanning instructions, administer contrast materials, prepare and operate the CT scan equipment and position the patient to capture the appropriate images. Taking into account that there are hospitals that use more than 100 different CT study protocols, it is expected that the technologist is proficient enough to follow them. When the scanning process is complete, the technologist must be in a position to evaluate CT scans for technical quality, collate processed images in sequence of exposure and appropriately label them. Furthermore, technologists handle the transmission and archiving of the digital scans that are produced, through the picture archiving and communication system (PACS). Since technologists come in direct contact with the patient, it would be useful if they received training on basic nursing and communication skills; for example, this kind of training could facilitate the co-operation of the patient in cases where the patient is experiencing significant psychological or physical discomfort / pain and a specific positioning is required in order to receive an informative image. Therefore, it is obvious that the technologist’s role is a key position in the CT scan workflow. The fact that the technologist handles so many different components and equipment during the CT scanning process allows for significant room for improving the quality and speed of the service provided. The less experienced or properly trained a technologist is, the more errors are expected, which results in repetitive scan referrals by the physicians.
Boland (2008) suggests that increasing the CT scan capacity (without purchasing extra equipment) would require a thorough workflow analysis, in order to identify the areas, where inpatient and outpatient CT throughput can be improved. The author highlights that professional development of technologists (radiographers) can have a significant impact on reframing the workflow and provides several valid suggestions for increasing the CT scanner capacity by investing in the further education of CT technologists. Although the presence of a radiologist is important in a CT scanning platform, technologists can be trained by a radiologist to recognise some common and easily identifiable patterns, such as liver lesions, which may require additional scans for characterisation. Traditionally, in these cases a radiologist would have to review the scan and request additional imaging. By training the technologists to recognise at least a limited number of such cases, they could perform the additional scan straight away without wasting extra slots and resources, while waiting for the radiologist to approve a repeat scan. Boland (2008) believes that while radiologists should be available in order to answer immediate questions from the patient or the technologist (or in cases that the patient has an adverse reaction to the contrasting agent), being removed from the scanning process itself as much as possible, would undoubtedly improve the patient throughput. The adherence to a standardised disease-specific CT protocol can significantly speed up patient throughput as well. Such a protocol would be implemented by radiologists, while technologists will be properly trained and subsequently able to use the correct protocol according to the clinical indications of the patient. Finally, technologists can be trained to use more efficiently the various IT platforms used in their department. Branstetter (2007) insists that CT technologists should have a good understanding of the radiology imaging technology and communication platforms, so that they can do their job efficiently and correct the quality of the pictures when necessary. This would result in faster patient throughput and it would also minimise overexposure of the patient to radiation.
Waaler and Hoffman (2010) report that although digital imaging technology has reduced dramatically the overall reject/retake percentage, the rejections due to operational incompetence (i.e. positioning errors) have remain unchanged or increased slightly. Foos et al. (2009) studied a significant number of scans from two different hospitals and found that almost 5% of the examined scan records were rejected by the technologists themselves because the quality of the image was unsatisfactory. The most common reasons for rejection of CT scans images were improper positioning / anatomy cutoffs (an average of 50%) and exposure errors (average of 13.5%), all of which indicate operational errors. These mistakes resulted in repetition of the scan. The authors found that in some cases (mainly in overexposures) contrast-brightness adjustments could have produced an informative image, saving time, productivity and the need to expose the patient to extra radiation (after having received a higher dose already). Jones et al. (2011) found that positional errors were responsible for more than 70% of the repeated images taken on a monthly basis.
Sanelli et al. (2007) on the other hand measured the effect of training and experience in CT perfusion data. The authors found that the most inexperienced (junior) CT technologists benefited the most by the additional training and were more confident in assessing qualitative and quantitative data. Similarly, Pierce et al. (2012) found that after a three-month training period, the error rates were reduced by almost 50%, while the proportion of examinations completed within four hours was significantly increased. As with the previous study, the authors found that the most inexperienced technologists improved the most. In-house training of CT technologists in the NHS context has been successfully implemented in many cases, leading to a significant increase in the CT scanner capacity. Case studies from the NHS Improvement in Diagnostics Scheme (2005) provide such examples, which resolved specific dysfunctional aspects of the CT service that used to lead to very long waiting lists. For example, the CT department of the Great Western Hospital did not provide a 24-hour service for stroke and urgent CT scans because the contracted night technologists were not qualified to perform them. Four training sessions provided by a senior radiographer dramatically increased the response time and improved patient care. North Cheshire Hospitals Trust NHS reduced the waiting time from five to two weeks within a month, by fully training their technologists for head CT scan reporting. This simple intervention increased CT scan capacity and allowed radiologists to handle more complex radiology tasks. In the Royal United Hospital in Bath, the training of two technologists in preparing and proper positioning of the patient, as well as a supplementary course in IV cannulation, resulted in a significant increase in the CT scanner capacity.
According to the Standards of Proficiency for Radiographers (2009) described in the Health & Care Professions Council (HCPC), upon his/her professional registration, a radiographer (or technologist) is minimally expected to be able to perform a standard head CT scan and only assist in other CT examinations, such as abdomen, chest and spine in acute trauma. Therefore there is plenty of room to improve the skills of technologists, who are prompted to extend and develop their skills further. Besides, in order for a radiographer to maintain his/her registration by HCPC, it is mandatory to undergo regular CPD programs. The NHS career progression framework recognises specific levels of practice related to service delivery. While the initial stage of technologists is referred to as practitioner, through continuous professional development the levels of advanced and eventually consultant practitioner can be reached, which represents the leading edge of the specific profession.
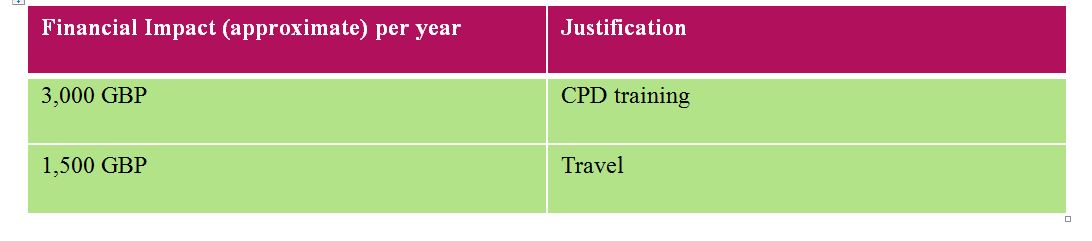
Financial Impact
The Estimated cost for one CPD event per annum for three CT technologists (minimum number of radiographers for operating a CT scanning platform on a 24-hour basis). Travel expenses applicable only for conventional study modules.
Evaluation
Supporting CPD and career progression for technologists is perhaps one of the most cost-efficient investments a radiology department could make. Experience with similar projects in NHS, proves that the effect on the CT scan capacity and quality of service can be immediate and long-term. As long as the employer recognises and supports Protected Time Study Agreements, the technologist can expand his/her skills according to the needs and services provided by the department and add great value to the existing service platform. Good collaboration between the technologist, the clinical provider (employer) and the education provider will make the whole CPD process smoother and more efficient.
The technologist can access CPD educational materials online (distance or e-learning) or enroll for a study day or other attendance-based programme offers. In order to facilitate the learning process, a variety of different settings should be encouraged. For example, informal and work-based learning can play a decisive role in efficiently applying and reinforcing the new skills. Opportunities for interprofessional learning (in conjunction with radiologists) and appropriate mentorship can also play an important role. The learner should have access to a range of resources in order to support the learning process, such as access to library and Internet access to relevant electronic journals. Some of these resources may be available by the institution providing the education, but the employer could also contribute to this process as well. Participation to departmental CPD activities and clinical meetings can promote the learning of new skills even more and should be encouraged by the employer.
References
Boland G. (2008) Enhancing CT Productivity: Strategies for Increasing Capacity. AJR 191:1, 3-10
Branstetter B.F. (2007) Basics of imaging informatics. Part 1. Radiology 243:656–667
Clinical Imaging and Oncology: Learning and Development framework for clinical imaging and oncology. (2010) Society of Radiographers. Available at: http://www.sor.org/system/files/document-library/public/sor_learning_development_framework_clinical.pdf [Accessed 25.11.2012]
Daily Mail (2011) Hospital waiting times rocket as scrapping of targets leaves thousands waiting more than six weeks for key tests. Available at: http://www.dailymail.co.uk/health/article-2011911/Hospital-waiting-times-Scrapping-targets-leaves-16-000-waiting-weeks-key-tests.html#ixzz2Cyc77PwF [Accessed 22.11.2012]
Dickson N. (2009) At breaking point: the NHS funding crisis. Nurs Manag (Harrow). 16(8):11.
Foos D. H., Sehnert W. J., Reiner B., Siegel E.L., Segal A. and Waldman D. L. (2009) Digital Radiography Reject Analysis: Data Collection Methodology, Results, and Recommendations from an In-depth Investigation at Two Hospitals. J Digit Imaging. 22(1): 89–98.
Grant L., Appleby J., Griffin N., Adam A., and Gishen P. (2012) Facing the future: the effects of the impending financial drought on NHS finances and how UK radiology services can contribute to expected efficiency savings. British Journal of Radiology 85, 784-791
Health & Care Professions Council: Standards of Proficiency – Radiographers. (2009) Available at: http://www.hpc-uk.org/publications/standards/index.asp?id=51 [Accessed 25.11.2012]
Imaging case study: Training radiographers to perform CT Heads. NHS. Available at: http://system.improvement.nhs.uk/ImprovementSystem/ViewDocument.aspx?path=Diagnostics%2fNational%2fWebsite%2fTraining_radiographers_CT_heads.pdf [Accessed 25.11.2012]
Jones A. K., Polman R., Willis C.E., and Shepard S. J. (2011) One Year’s Results from a Server-Based System for Performing Reject Analysis and Exposure Analysis in Computed Radiography. J Digit Imaging. 24(2): 243–255.
NHS Improvements in Diagnostics. (2005) Modernising radiology services: A practical guide to redesign. Available at http://www.improvement.nhs.uk/diagnostics/RadiologyKeyResources.aspx [Accessed 23.11.2012]
Pierce L, Raman K, Rosenberg J, Rubin GD. (2012) Quality Improvement in 3D Imaging. AJR Am J Roentgenol. 198(1):150-5.
Sanelli P.C., Nicola G., Johnson R., Tsiouris A.J., Ougorets I., Knight C., Frommer B., Veronelli S., Zimmerman R.D. (2007) Effect of training and experience on qualitative and quantitative CT perfusion data. AJNR Am J Neuroradiol. 28(3):428-32.
Sankaran A. (2009) Pocket-size solid-state iPOD and flash drives for gigabyte storage, display and transfer of digital medical images: Review and work initiated. J Med Phys. 34(3): 167–175.
Silvester K. and Steyn R. (2008) Why do we get queues and waiting lists? NHS
Tokur S., Lederle K., Terris D., Jarczok M., S. Bender S., Schoenberg S. and Weisser G. (2012) Process analysis to reduce MRI access time at a German University Hospital. Int. Journal for Quality in Health Care 24:1, 95-99.
Waaler D, Hofmann B. (2010) Image rejects/retakes–radiographic challenges. Radiat Prot Dosimetry. 139(1-3):375-9.