Essay on the Rise of Telemedicine
Number of words: 1683
Introduction
Telemedicine aims at improving a patient’s clinical health status through electronic communication where medical information is passed on from one site to another via this platform. Telemedicine is revolutionizing the way in which practitioners are delivering healthcare as well as how consumers are receiving it. The shortage of doctors in rural areas about four decades ago led to the increase in popularity for telemedicine (Mahar & Rosencrance, 2018). However, health monitoring during space flights for astronauts by the National Aeronautics Space Administration (NASA) 50 years ago led to the establishment of the concept of telehealth. There is a sense of inevitability to telemedicine rapid growth as a healthcare strategy due to great technological advancements in the recent past.
Advantages of telemedicine
- Store and forward. There is easy access to patient data through cloud-based technology including videos, photos, MRIs and X-rays. Dermatology, ophthalmology, pathology and radiology are examples of medical fields where this store and forward technology is commonly utilized.
- Employing medical information systems which are cloud-based, telemedicine facilitates the health industry to work as one. Separate visits to specialists are avoided by patients and this means that they save on cost and time. Clinical decisions can be discussed via email or video between doctors or other specialists as way of collaborating.
- For everyone, the preciousness of time cannot be overstated. Patients in any geographical location or time zone in the world can be ‘seen’ by a medical practitioner through computers, tablets and smartphones which enable access to the cloud. This technology comes very handy for patients who face difficulties in accessing transportation to a treatment or clinic facility or those who generally have mobility challenges (Ohannessian, 2015).
Problems associated with telemedicine
Implementation roadblocks exist for both patients and the health industry despite the obvious adoption benefits of telemedicine. The challenges include:
- The sensitive nature of healthcare and its data cannot be overstated. The telemedicine industry faces the risk of breaches and cyber-attacks that would compromise the security of patient’s data.
- Compatibility of equipment. Ecosystems of telemedicine can be intricate. There is a high likelihood of devices malfunctioning with servers, gateways, SBCs and other multiple pieces of equipment. Increase in the possibility of incompatibility is realized when devices are replaced or upgraded.
- Dropped connections. An internet connection that is both stable and can operate in high speeds is crucial. Reliability of the devices used for communication is paramount. Having to deal with glitches due to poor internet connection is a disservice to physicians who normally have heavy workloads. Missed instructions and potential mismanagement of a patient might result from an interrupted connection between a patient and a physician which might not necessarily be an issue if the conversation was personal.
Surmounting the challenges
People are not the only ones who undergo health checks. Maximum performance and good shape for communication ecosystems and technology should be regularly ensured by the healthcare institution. Telemedicine industry success is usually based on performing constant troubleshooting and network monitoring. This is crucial just as the technology and equipment. The user infrastructure is under threat if there are no tools to correctly predict future problems or tools to address the aforementioned challenges immediately.
Telemedicine impact in the fight against Coronavirus (COVID 19)
Up until the declaration of Coronavirus as a pandemic by the World Health Organization (WHO), the success story that telemedicine hoped to realize was just a mirage. The technology promised to make waiting in line for hours a thing of the past through the access of state-of-the-art healthcare while also showing signs of being at the forefront of medicine’s future. For many, however, the technology was merely a concept that was only adopted by a few regions and countries. Only 18% of consumers in the United States used telemedicine services according to a study. Lack of awareness and proper infrastructure could be attributed to such a sad state of affairs. Like it is commonly the case in digital health, cultural aspects are not accounted for. Additionally, the effectiveness and reliability of telemedicine has been questioned by would-be consumers (Bashshur, 2020).
But then again, the Coronavirus (COVID 19) pandemic struck. Every aspect of society has been severely disrupted COVID 19; from the way we work, the rhythms of our personal lives, our collective levels of anxiety as well as the well-being of our society. Due to the need of limiting exposure to the virus, healthcare providers had to find alternative ways of offering their services. Ideally, the use of telemedicine reduces the spread of the disease, offers healthcare institutions with the opportunity of prioritizing important cases by limiting patient displacement to hospitals. The extent of COVID 19 and its effect on society could not be predicted just a couple of months ago. In order to curb the spread of the virus, lockdown measures have been imposed in numerous countries across the world. In these unprecedented circumstances, an adequate solution is digital health (telemedicine). The healthcare industry is increasingly adopting remote consultation as the work-from-home solution is being implemented in schools and even in companies. Telemedicine technology was brought into a new light due to the Coronavirus pandemic. The remote technology need went through the ceiling as physicians needed to remain disease-free and stay healthy. When patients travel to the hospital, they run the risk of spreading the virus and therefore telemedicine is being recommended by the WHO as the best way to monitor patients. A telemedicine company CEO, Said Dedi Gilad asserts that, “The gap between health systems, doctors and patients is being bridged by telemedicine, enabling doctors through virtual channels to communicate with particularly symptomatic patients from the comfort of their homes and thereby assisting to arrest the spread of Coronavirus to the masses and other frontline workers.” Under the threat of COVID 19, the significance of telemedicine is well summarized by the quote from Dedi Gilad.
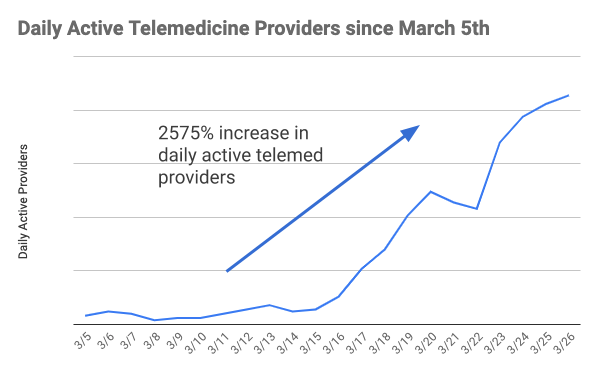
In the United States, the number of telemedicine providers surged exponentially in a 30-day period in March, 2020.
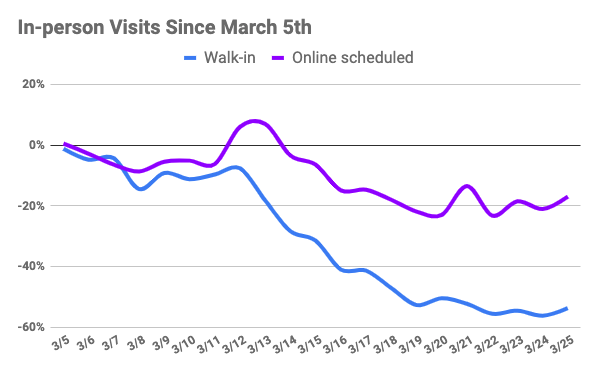
Still in the United States, unsurprisingly, there was a 57% decline in walk-in patients while there was a 17% drop in patient numbers who schedule their visits in advance.
The most unfortunate bit about telemedicine is the potential for fraud that comes with it. Individuals who are not tech savvy, especially the elderly mostly find themselves on the receiving end of this type of fraud. A litany of fraud schemes were launched in the wake of Coronavirus pandemic by unsavory players in the healthcare industry. Complexity of visits and time inflation through upcoding and overbilling are the main fraud schemes. Furthermore, billing for durable medical equipment (DME), tests and unnecessary services as well as billing for services never rendered represent additional avenues for fraud.
May be in Post-COVID 19 the bubble being experienced by telemedicine will finally burst. Currently, its growth is being stifled pricing and regulation issues. Telemedicine might go back to oblivion as it awaits the next pandemic. Nonetheless, a health crisis of global proportions may take place again. Coronavirus, Zika Virus, Ebola and MERS have all been observed in less than a ten years. Key stakeholders should recommend that healthcare systems embrace telemedicine since it has demonstrated its importance especially in the current unprecedented times (Portnoy et al., 2020).
Job implications of telemedicine
Positive implications
Rural and underdeveloped regions of the globe are set to benefit from E-consults and E-visits where secure phone or email encounters are used by doctors to communicate with patients. A wider pool of specialized doctors is availed to the rural people who would otherwise not get access to these services. For the doctors, the more the clients they attend to per day the more they get paid. This represents an avenue where physicians can make a lot of money. For doctors and nurses, traditional requirements of time and location are not observed in this system thereby offering flexibility. A reliable and fast internet connection is all it takes for them to provide medical care to their patients (Roberts & Mehrotra, 2020).
Negative implications
A lot of time and money is expended when purchasing new equipment and restructuring the IT personnel responsibilities. An effective telemedicine program can only be built when there is sufficient training for all the staff involved, e.g., practice managers and doctors. Moreover, there might be a decrease in staffing requirements. For example, with the help of telemedicine, over 30 patients can be monitored by a single nurse simultaneously from any part of the world. With the advent of robotic devices in surgeries, the staff members involved are considerably reduced. To facilitate less invasive surgeries, video cameras are being utilized. Rather than open the patient completely, the camera is accommodated via small incisions. The cameras are controlled by the robotic devices while at the same time the devices act as the surgeon’s arms. Surgical assistants would be become redundant as the robots take over their jobs (Makhni et al., 2020).
References
Bashshur, R., Doarn, C. R., Frenk, J. M., Kvedar, J. C., and Woolliscroft, J. O. (2020). Telemedicine and the COVID-19 Pandemic, Lessons for the Future.
Mahar, J. H., Rosencrance, J. G., and Rasmussen, P. A. (2018). Telemedicine: Past, present, and future. Cleve Clin J Med, 85, 938-942.
Makhni, M. C., Riew, G. J., and Sumathipala, M. G. (2020). Telemedicine in orthopaedic surgery: challenges and opportunities. JBJS, 102, 1109-1115.
Ohannessian, R. (2015). Telemedicine: potential applications in epidemic situations. European Research in Telemedicine/La Recherche Européenne en Télémédecine, 4, 95-98.
Portnoy, J., Waller, M., and Elliott, T. (2020). Telemedicine in the Era of COVID-19. The Journal of Allergy and Clinical Immunology: In Practice, 8, 1489-1491.
Roberts, E. T., and Mehrotra, A. (2020). Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA internal medicine, 180, 1386-1389.