Essay on HIV
Number of words: 3284
The human immunodeficiency virus (HIV), was discovered by Barré-Sinoussi, Montagnier and their colleagues at the Institute Pasteur, Paris, in 1983 (1). HIV is a part of the genus lentivirus (a subgroup of retrovirus), and member of the family Retroviridae (2). The virus has two distinct types that cause AIDS; HIV-1, which has four groups M, N, O and P. This strain is responsible for the majority of infections worldwide (95%). And HIV-2, which is concentrated in West Africa, and is less infectious and has a slower progression rate than HIV-1. Since its emergence, HIV has caused a total of 35 million deaths and infected 76.1 million individuals, one of which being Andrew, whom this case study is focused on.
HIV consists of a cylindrical centre which is surrounded by a lipid bilayer that is sphere shaped. The two major types of viral glycoprotein are gp120 and gp41, which function as mediators for the recognition of CD4+ cells and chemokine receptors. Thus, allowing the virus to attach to and invade CD4+ cells (3). The inner sphere contains: two single-stranded copies of the genomic material (RNA); enzymes and proteins required for the replication and maturation of HIV. A feature that is unique to HIV is that unlike other retroviruses, it uses nine genes to code for the necessary proteins and enzymes. The gene ‘gag’ encodes core proteins, ‘pol’ encodes the enzymes reverse transcriptase, integrase and protease. ‘Env’ codes for the glycoproteins and the rest of the genes are needed for its replication and infectivity rate (3).
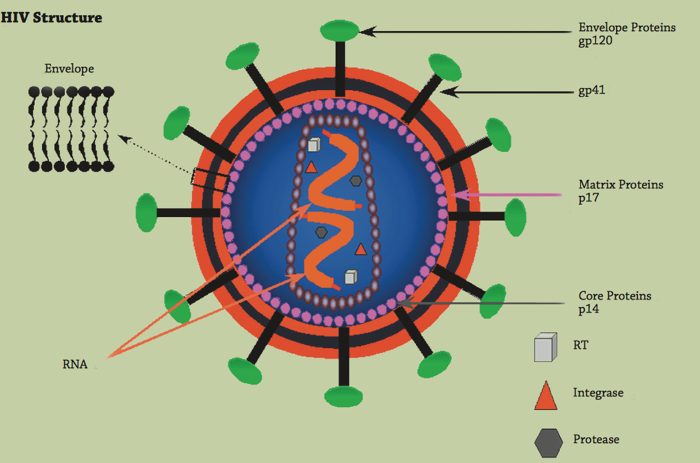
Image showing the structure of HIV (3)
The development of HIV is dependent on the battle between the virus’ replication, and the individual’s immune response via the cell and immune mediated reactions (3). Host cells that have been infected with HIV have a shortened life span, this is because they are used as ‘factories’ to replicate (3). During the first day (after exposure), HIV either attacks or is captured by the dendritic cells in the mucous membranes (3). The infected cells then migrate to the lymph nodes and then the peripheral blood. There are six phases in the HIV life cycle: binding and entry, reverse transcriptase, integration, replication, budding and maturation. In binding and entry, the gp120 and gp41 (envelope proteins) bind to CD4+ cell receptors and also coreceptors outside of the CD4+ cells and macrophages. CCR5 and CXCR4 are chemokine receptors that facilitate the viral entry. HIV tropism require CXCR4 to bind and macrotropic strains require CCR5. The joining fuses the HIV membrane with the CD4+ cell membrane. As the virus enters, the membrane and envelope proteins remain outside of the CD4+ cell, however the core enters. The enzymes of CD4+ interact with the viral core and stimulate viral RNA and enzymes reverse transcriptase, integrase and protease to be released (3). Reverse transcriptase then converts HIV RNA to DNA, this must happen so that it can be incorporated into the CD4+ DNA and multiply. The single strand of DNA is replicated into double-stranded HIV DNA. After, integrase inserts viral DNA into CD4+ cells’ DNA (in a process called integration). Replication takes place after this, causing the production of mDNA that initiates the synthesis of HIV proteins. After budding, maturation take place, in this stage the mature virions bud from the infected host cell, once they’re in free circulation the cycle begins again (3).
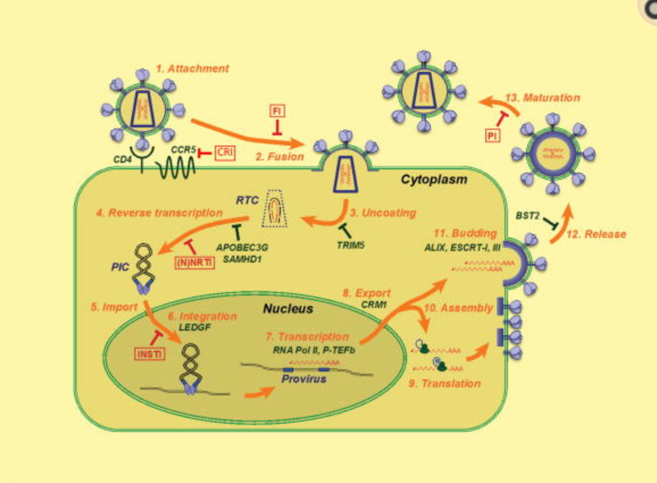
This image clearly shows the stages of replication of HIV (4).
Transmission of HIV formerly occurred via blood transfusions (factor VIII for haemophilia A), however, due to the development of screening, the risk of this is presently low (5). Vertical transmission of HIV (mother to infant), is the third most common way in which HIV can be transmitted globally. This can occur during pregnancy, delivery or breastfeeding. Horizontal transmission occurs through contact with body fluids (semen, pre-seminal, vaginal and rectal fluids) via unprotected oro-genital intercourse and also infected blood. Transmissibility varies between the transmission’s routes; unprotected anal sex has the greatest risk and then vaginal (5). Transmissibility also varies according to the different infectiousness and susceptibility of the individual. It is greatest during the earliest and later stages of HIV, which is before the antibodies are produced or once AIDS has occurred. Co-factors such as other STDs (chancroid) can amplify the transmission (5). Regarding this case study, Andrew, is most likely to have contracted HIV from his numerous homosexual relations prior to his marriage. He was likely to have had anal sex without using protection or any medication to prevent HIV, this is known as pre-exposure prophylaxis. Aside from the biological factors that initiate HIV, social institutions also play an important role. Social discrimination and homophobia make it difficult for them to access health care. This creates more risks in Andrew’s case as he could have transmitted the infection onto his family
HIV has three stages: acute HIV infection (patient develops flu-like symptoms); chronic HIV infection (asymptomatic and latency period) and acquired immunodeficiency syndrome (AIDS). People with HIV are diagnosed with AIDS if their CD4 count is less than 200 cell/mm3 or they have more than one opportunistic disease, such as cervical and blood cancer, Kaposi’s sarcoma and infections like herpes and candidiasis (6). The Walter Reed staging system of HIV infection classifies patients on the basis of CD4 counts, skin-test responsiveness, lymphadenopathy, oral candidiasis and opportunistic infections (7). The progression to AIDS is dependent on a number of factors; the viral ‘set point’, route of transmission, age and ethnicity. HIV progresses to AIDS after a median of 11 years, however, its rate is very variable. On one hand, there are long term survivors that are free of clinical AIDS after 20 years and there are also those who manifest AIDS and die within 2-3 years (6).
Diagnosing HIV has changed immensely since its inception in 1980s, due to their sensitivity enzyme immunoassays (EIA) can detect HIV antibodies one-two weeks after contraction. EIA are commonly used to screen for infectious diseases, however, they can produce a false positive result. Thus diagnostic laboratories often confirm positive EIA tests with another assay (8). Western blot is usually the confirmation assay used, it is an immunoblot that tags the antibodies to each viral protein. The individual’s serum is reacted with a nitrocellulose strip which has the HIV virus proteins. If the patient’s serum contains any specific antibodies it will bind to the antigen and a coloured band is formed (8). Moreover, p24 antigen is a distinctive HIV viral protein that makes up most of the viral core. Newly infected individuals have high levels of p24 in their serum, thus making p24 antigen assays useful in primary HIV diagnosis. Furthermore, due to its ability to pick up small numbers of viral particles, PCR is also used, particularly in vertical transmission (8).
The treatments for HIV are dependent on the stage of the disease and any associated opportunistic infections. Effectively, the goal of the treatment is to prevent the immune system deteriorating so much that the individual develops opportunistic infections. The current HIV treatments can reduce: HIV-associated morbidity; survival and transmission of HIV. All viremic patients are recommended Antiretroviral therapy (ART) during the acute infection period, irrespective of their CD4 count. This reduces the size of the latent HIV reservoir and immune activation prior to development of positive HIV antibody. Reverse transcriptase inhibitors along with integrase and protease inhibitors all affect the HIV-1 Enzyme. HIV uses a compound called reserve transcriptase (RT) to convert its RNA to DNA. RT inhibitors include nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs) i.e. Abacavir, these were the first type of drug available to treat HIV. They work by blocking RT enzyme, this prevents the infected cells making more HIV. Non-nucleoside reverse transcriptase inhibitors (NNRTIs) i.e. Delavirdine is also used. These bind to specific protein, thus preventing replication. Additionally, HIV-1 protease inhibitors such as Amprenavir are peptidomimetics that bind to the enzymes active site and prevent new HIV becoming mature. An advantage of this is that they are not susceptible to proteolytic cleavage, due to the presence of hydroxyethylene bonds. HIV-1 integrase inhibitors or integrase strand transfer inhibitors are also another form of treatment. They work by stopping HIV making copies of itself by blocking a protein that enables the virus to insert its DNA into healthy cell’s DNA. Enfuvirtide injection is an entry inhibitor, entry inhibitors are divided into two types: inhibitors of viral and cell membrane fusion and inhibitors of the binding of viral envelope proteins to receptors. This class of treatment works differently to PIs, NRTIs and NNRTIs, which are active against HIV after it has infected a CD4 cell. EIs and also fusion inhibitors work prior entry, thus would benefit patients who have become resistant to the other types. CCR5 antagonists such as Maraviroc prevent HIV entering a CD4 cell by blocking a ‘hook’ on the outside of the cell and disabling the virus plugging in (9).
In 1995 a combination drug treatment which was at the time known as ‘AIDS cocktail’ was discovered, it had two inhibitor types which targeted different sites of a single enzyme (9).
This drug is presently referred to as Highly Active Antiretroviral therapy (HAART) or Combinational Antiretroviral therapy (cART). It was introduced as a result of failure of the drug AZT, when HIV mutated and became resistant to the monotherapies. Since its emergence, HAART has led to dramatic improvements in HIV positive patients (10). There has been a decrease in the amount of HIV in their bodies and an increased CD4 count. Apart from benefitting the individual, HAART has also been successful in reducing the acquisition and transmission of the virus (10). A combination of three or more inhibitors (NRTIs, NNRTIs and PIs) reduces the dose of each of them, thus increasing the efficiency due to the simultaneous action on the HIV and reduces the chances of resistance which is present in 10-15% of patients (9).
As well as the virologic response, treatment of opportunistic infections is paramount and should be directed at. Although effective ART reduces the risk of the progression and transmission of HIV and its related diseases like Kaposi sarcoma, it brings with it many adverse effects. Some of the common effects include gastrointestinal complications like nausea and diarrhoea which can continue throughout the entire course of therapy (11). However, there are more serious adverse effects like HIV lipodystrophy that can accompany ART. HIV lipodystrophy or fat maldistribution is a syndrome that refers to abnormal central fat accumulation (lipohypertrophy) and localised loss of fat (lipoatrophy), it is also cosmetically disfiguring (11).
Discrimination is manifested due to stigma. Stigma has a historical foundation and has consequently led to a destabilization in the social structure. Although most diseases possess a certain degree of social stigma, one of the most tragic cases of discrimination has been towards HIV and AIDS; this is known as serophobia. It is ironic that in an age, where medicine and technology are rapidly progressing there are numerous social issues of hostility and rage towards those with the disease. The stigma carries the inherent identity of dividing people into groups (12). Much of the prejudice involves homosexuality, sex workers, promiscuity and those with illegal intravenous drug use. Furthermore, it has had a catalytic role in the mistreatment of pregnant women, specifically in third world countries. HIV-positive pregnant women often experience depression as they feel guilty and responsible for being sick. In addition to this, affected individuals are often excluded from job opportunities and in some cases prohibited from basic human rights of consent or confidentiality (being forced to take HIV tests) (12).
Although it is unethical, some doctors have in the past refused treatment of HIV patients. Successful management of HIV involves addressing the patient’s social needs as well as their medical. Therefore, a supportive patient-doctor relationship is crucial. Medical and scientific groups are often blamed for lack of education they provide to communities, meaning ignorance often takes control of their actions. The fear of isolation has meant that people currently with HIV have delayed the initiation of their treatment; this not only increases the risk of morality but also transmission onto people around them (12). Moreover, the intervention of media and education have decreased HIV/AIDS discrimination; digital technology, cultural exposure and personal experiences significantly effect society’s attitudes, this may be because by publicly talking about it, it normalises the concept (12).
Although the personal information disclosed by Andrew to his physician may be of interest to his pregnant wife and children, due to confidentiality being an unwritten ethical obligation, this cannot happen unless Andrew himself gives permission. This is a controversial topic, as on one hand it can be argued that the patient has a legal right to privacy and on the other hand those who can be potentially affected also have the right to get tested and commence treatment. Andrew has to carefully consider the repercussions of his choice. As his wife and children can be infected through sexual intercourse and vertical transmission. Although HIV is not a disease that can be legally disclosed to the patient’s family, Andrew’s doctor may choose to inform his wife once he develops an opportunistic infection that can be legally disclosed (like pneumonia), given that he refuses treatment.
The mechanism in which science communication takes place is continuously changing. It is becoming easier for critical information to spread to communities that have traditionally been excluded from the process of science. As well as that, it plays an important role in fueling controversies, like what happened in the case with Woo-Suk Hwang. Irrespective of the obstacles and drawbacks that scientists and their articles face, their discoveries and knowledge is at the heart of society’s progression.
In AIDS-related medical and social situations, the right to free oneself from discrimination has received great attention. Stigma is a multifaceted social structure that has its own pathway; it starts with labelling, separation, status loss, and ends up in discrimination. It is known that the impact of vulnerability and sensitivity to stigma differ from person to person. The main goal of modern medicine is to eliminate stigmatization and discrimination and to ensure confidentiality in testing and counselling.
Reference List
- Adler, WM (ed). HIV and Related viruses. ABC of AIDS. 5th ed. London: BMJ Publishing Group. (2001). pp.7-8.
- Wikipaedia contributors. HIV. Wikipaedia. 2018 Nov. p1-2. Aids.gov.hk.
- Calles Rn, Evans D, Terlounge D. Pathophysiology of the human immunodeficiency virus. HIV curriculum for health professionals. 2009:13: 7-12.
- Engelman A, Cherepanov The structural biology of HIV-1: mechanistic and therapeutic insights. Nat Rev Microbiol. 2012 Mar 16; 10(4): 279–290.
- Bloor M. The sociology of HIV transmission. Guildford. SAGE publications. 1995. P7-8.
- Naif Pathogenesis of HIV Infection. Infect Dis Rep. 2013 Jun 6; 5(Suppl 1): e6
- Redfield RR,Wright DC, Tramont EC. The Walter Reed staging classification for HTLV-III/LAV infection. N Engl J Med. 1986 Jan 9;314(2):131-2.
- Meulendyke AK, Croteau DJ, Zink HIV life cycle, innate immunity, and autophagy in the central nervous system. Curr Opin HIV AIDS. 2014 Nov; 9(6): 565–571.
- Prokofjeva MM,Kochetkov NS, Prassolov Therapy of HIV Infection: Current Approaches and Prospects. Acta Naturae. 2016 Oct-Dec; 8(4): 23–32.
- Brechtl JR,Breitbart W, Galietta M, Krivo S, Rosenfeld B. The use of highly active antiretroviral therapy (HAART) in patients with advanced HIV infection: impact on medical, palliative care, and quality of life outcomes. J Pain Symptom Manage. 2001 Jan;21(1):41-51.
- Montessori V,Press N, Harris M, Akagi L, Montaner Adverse effects of antiretroviral therapy for HIV infection. CMAJ. 2004 Jan 20; 170(2): 229–238.
- Kontomanolis NE, Michalopoulos S, Gkasdaris G, Fasoulakis The social stigma of HIV–AIDS: society’s role. HIV AIDS (Auckl). 2017; 9: 111–118.