The Multidisciplinary Approach to Medicine
Number of words: 9340
Introduction/Background
A multidisciplinary care team is a group of healthcare workers that includes doctors, nurses, respiratory therapist, CNAs, dietitians, primary care physicians, and administrators, other specialists who collaborate within their healthcare institution to offer high-quality, integrated treatment to patients. For long-term patient care, multidisciplinary teams are becoming more prevalent, in order to serve patients with severe and other illnesses with high-quality, customized treatment (Healthie INC, 2021). One may handle the complete patient as well as provide effective healthcare by collaborating with a multidisciplinary team. With each professional focusing on a distinct element of the patient’s health, practitioners are more likely to discover areas of need and address those needs effectively. Inside the healthcare institution, multidisciplinary care promotes efficiency and saves a lot of time. Attempting to deliver care throughout a healthcare sector without teamwork can result in miscommunication and mistakes in patient safety. It has been proven that working as part of a care team reduces service duplication, and to prevent such incidents, tasks are properly explained and allocated to participants. (Healthie INC, 2021).
Statement of the Problem
Communication process between doctors, managers, and executives in a major healthcare institution may be a difficult process. Members may be unable to interact with one another on a daily basis due to different departments, shifts, and scheduling, regardless of how important teamwork is inside a company. To guarantee that your team’s patients receive the best possible care, team cohesion may be improved by using internal communication techniques. The first and most crucial stage is to establish open lines of communication between providers According to research, organizational communication in which all individuals engage in discussion, is becoming increasingly prevalent, rather than one-sided interactions from a supervisor or administration. (Healthie INC, 2021). Multi-Disciplinary Meetings (MDM) are gatherings in which medical and allied health care experts discuss pertinent alternatives and reach a consensus on a diagnosis. It has been discovered that prognosis or therapy for a patient leads to greater judgments than choices taken only by specialists. (Sharma et al., 2016).
Purpose of the Study
The purpose of the study is to conduct a comprehensive medical literature review to assess the impact of multidisciplinary teams in medicine and their efficacy in terms of patient care, duration of stay, successful results, and safety.
Rationale
Multidisciplinary teams are relatively new in healthcare. However, physicians, administration, nurses, etc. are aware of multidisciplinary teams, but it is not always implemented. Every facility has a different way of doing things and communication is always something that needs to be worked on. By researching the literature and analyzing data and trends, I can provide facilities and practitioners with the information they need to make effective decisions.
Significance of the Study
My personal experience with the multidisciplinary approach to medicine is that it created an efficient and collaborative work environment and an all-around better experience for the patient. The point of this approach is to have proficient communication and productive outcomes for the patient. This approach benefits everyone in the hospital, from administrators, CEOS, nurses, respiratory therapist, CNAs, and patients. To deliver effective and safe healthcare services, it’s vital to operate as a team. Patient satisfaction, nurse retention, and hospital expenses are all improved in hospitals that have high collaboration scores. (O’Leary, 2012).
Literature review
Multidisciplinary teams are a method of arranging and merging health-care services in order to meet the needs of persons with complex medical problems (science organization UK, 2021). The teams combine the understanding and information of a variety of professions to assess the situation as a whole, coordinate, and manage care. According to science organization UK, 2021 Multidisciplinary teams are designed to collaborate successfully in order to meet the needs of people, because they are community-based and linked to primary care.
By getting a variety of health services, multidisciplinary teams focus on keeping patients healthy and independent, healthcare, as well as other welfare services and administering the correct care at community – based settings and home, to avoid unnecessary hospitalization (science organization UK, 2021).
As healthcare systems have gotten more complicated, the establishment of these teams has become necessary. The many factors that influence patient outcomes necessitate the participation of experts from many fields. Most organizations that care for the severely sick have adopted multidisciplinary patient rounds as a standard practice. Other national healthcare bodies, as well as the World Health Organization, has developed treatment models and professional practice standards that use a multidisciplinary team as the therapy framework.
In many Intensive care units, you may witness examples of these teams at work. The social service, intensivist/physician, nursing, respiratory therapy, a pharmacist, and, if appropriate, a member of the family or the patient, make up the team. The diagnosis, presentation, and course of the patient are all reviewed by this team. The results of lab tests, diagnostic findings, medicines, and psychological issues are all addressed in a group setting. This is a great time to look for changes in the patient’s condition and go through the treatment plan and discharge options. Depending on the institution, this activity may happen once a week or every day. Researchers and undergraduates from a variety of fields are welcome to attend to participate in some facilities as a teachable moment.
Each team member contributes something unique. The healthcare professional will usually begin by introducing the patient and discussing his or her medical background. Nursing provides a bedside perspective on the patient’s condition, medicines, discomfort, and psychological issues. This gives pharmacy the opportunity to express concerns about prescription orders or usage; therapeutic response and pulmonary care status will be addressed by respiratory therapy; and Performance, response to therapy, and the willingness to continue will be discussed by physical therapy. All of data is used by social work, and the team may discuss the discharge plan, the patient’s and family’s wishes, and any assistance that they may be eligible for. As the talk develops, the patient and family may raise questions.
The patient, the healthcare team members, and the organization are the three essential stakeholders in the team. Improved results, shorter hospital stays, fewer ventilator days, and better communication with all caregivers benefit the patient. Coordination of different providers is critical to achieving favorable results, and this is especially true in complicated care management circumstances. The utilization of a multidisciplinary team also gives the patient and caregiver a voice in the treatment of the patient.
There are several advantages for healthcare professionals. Since communication is real-time and interactive, the team can enable clinicians to look at patient care and results strategically. Not only can this be used to respond to crises, but it can also be used to initiate long-term planning and prevention. Multidisciplinary teams have been found to increase professional happiness, increase provider knowledge, and stimulate creative thinking among experts.
The advantages for the healthcare organization are purely financial. Better outcomes, shorter lengths of stay, lower healthcare costs, and fewer staffing and bed management responsibilities are all benefits of enhanced care quality. Additional advantages include increased patient satisfaction and a better reputation in the community.
Open-minded learning, communication, and mutual appreciation for what each discipline brings to the table are the keys to success for a team like this. Unfortunately, several businesses only pay lip service to this process, relying on forms and formats that describe procedures and satisfy standards but aren’t genuinely interactive. Face-to-face connection is desired, though it is not always possible; nevertheless, in today’s tech-savvy society, essential conversations may now be conducted online as well.
There ought to be a specific objective in mind for a multidisciplinary team to be successful. To sum up that, Multidisciplinary Teams must have a clearly delineated function that demands members of the team to collaborate across professional and disciplinary lines. The multidisciplinary team’s goal must be communicated clearly for each member of the team to comprehend.
Institutional support is critical to the effectiveness and success of a multidisciplinary team. Employing organizations and (if in situ) partnering entities governing this area of partnership should give assistance. Obtaining support from the public should be a part of this (and therefore credibility), guaranteeing the multidisciplinary teams have the instruments they require, and performance management metrics are being developed.
The importance of team leadership in a multidisciplinary team cannot be overstated. Leaders must use a positive and constructive attitude in order to promote diverse contributions, but they should also be directive when required. A team leader’s knowledge of team dynamics and readiness to criticize bad interprofessional collaboration are essential skills.
Prospects for collaboration in multidisciplinary team are expected. Multidisciplinary teams require physical time and space to accommodate participants from a variety of professions and specialties. This improves communication and allows them to better comprehend each other’s responsibilities and skills.
Before focusing the patients need, a people-centric healthcare facility has a culture that prioritizes workers and their behaviors, as well as internal and external customer service interactions. A multidisciplinary team faces a serious challenge from a people-centric institution. There’s a risk that teams grow overly focused on themselves and how they work. Families and communities may feel more alienated from talks about their care, rather than less.
Diverse roles are very important in a multidisciplinary team. In Multidisciplinary teams do not have a magical solution. Instead, the combination of specialties and professionals must cater to the requirements of the target community while remaining modest enough for participants to get to recognize one another.
Evidence-based healthcare is the deliberate, clear, and thoughtful application of current best evidence in making choices regarding individual patients’ care. Teams should be prepared to illustrate their overall impact in a manner that is both timely and precise. Providing planned opportunities for a team to reflect on the results is one of the most productive methods to enhance their performance.
What Role do MDTs Play in Integration?
Multidisciplinary teams are made up of professionals and practitioners from the healthcare, therapy, and related industries who collaborate to deliver comprehensive, person-centered, and integrated support and care. Multidisciplinary teams can comprise a variety of people, based on the delivery strategy and context. Link workers or care navigators are frequently included in multidisciplinary teams, and they may help in social prescribing by connecting people with local groups and community support services.
The synchronization of various actions and services, based around the multidimensional continuum of human problems, desired results and personal strengths is required for an integrated and holistic approach to support and care. Multidisciplinary Teams are critical in transcending professional divides and building bridges created by contending cultural and organizational variances. When they work, they make it possible to provide extensive, ongoing, and flawless healthcare.
MDTs, which are overseen by a designated care coordinator or leadership, can provide tremendous value towards service users. Multidisciplinary teams are now a more common technique for lengthy healthcare delivery, as they provide positive, tailored care to patients suffering from chronic and other illnesses. When dealing with patients, every other team member must not only have experience and competence, but they must also be capable of working cooperatively and efficiently with the other team members. When it comes to hiring, coaching, and communicating with a team of professionals, team leaders must be careful and precise.
The healthcare facility can treat the full individual as well as provide high quality care by collaborating with a multidisciplinary team. When each expert is focused on a different element of a patient’s condition, Practitioners are much more able to identify and treat subcategories dire need of help. Each team member can interact with the patients in their field of expertise while also cooperating to offer suggestions that will improve health care. Patients, who were treated by a team of specialists at a specialized stroke unit, were significantly more likely to be surviving, autonomous, and within a year of their stroke, they were back at home, than a single practitioner according to findings.
Across the healthcare facility, Multidisciplinary care increases efficiency and saves time. Trying to offer care throughout a medical system without synchronization can lead to misunderstanding and ineffective medication, in addition to lost time. Working as part of a healthcare team has been shown to decrease service duplication by explicitly defining and assigning duties to members of the team.
Patients will be more satisfied if their healthcare systems enhance. They now have more accessibility to a multidisciplinary care team that can help them with all of their problems. They can relax knowing that the entire patient is being cared for. Clients’ treatment time and expense spent in health – care settings are also reduced through concerted and coordinated team healthcare, particularly in-home care. Patients spend a little less time having to wait for clinicians, addressing their requirements, and going through the treatment regimen because of team cooperation and properly articulated suggestions. Patients devote as little time as possible in the facility since tasks are outsourced across the multidisciplinary healthcare team, allowing them to focus on completing the treatment plan and improve their health and wellbeing.
Care teams not only make patients happier, but they also make caregivers happier. As a consequence of specific tasks and effective communication, members of the team express better job satisfaction. Providers that are able to cooperate with other providers and participate in the decision-making process feel like they are an important part of the team. Providers gain a better grasp of their colleagues’ roles and duties as a result of enhanced collaboration.
Approaches to Putting Together a Patient-Centered Multidisciplinary Care Team
Examine the requirements of your group of patients.
The first step in forming an effective healthcare team is to examine your patient population’s needs in order to identify physicians who can provide tailored treatment to their patients. Members of the care team should be specialists in their fields and able to give effective, specialized care that is tailored to the needs of your specific patient populations. Physicians on the team should also share a similar approach to patient care. Each team member must first want to deliver patient-centered care on their own before they can form a team of patient-focused clinicians.
The healthcare needs of your patient demographic may also influence the types of doctors you hire. Customizing your multidisciplinary care team to fit the requirements of your patients will enhance patient outcomes and satisfaction, improve team cohesiveness, and reduce time spent training and retraining new providers.
Make sure you’re in touch with your Multidisciplinary Care Team
Effective internal communication between physicians, supervisors, and administrators can be a difficult task in a large healthcare firm. Despite the necessity of collaboration inside an organization, different departments, shifts, and schedules often prevent people from engaging with one another on a daily basis. Internal communication can easily fall between the cracks, especially in healthcare, where the focus of communication strategies is on external contact with clients.
Use internal communication tactics to enhance team cohesion and offer the best possible care for your team’s patients. The most crucial stage is to establish clear communication channels between suppliers. Organizational communication that involves conversation among all members, rather than one-sided messaging from a supervisor or administrator, is becoming more widespread, according to research. Make a team chat so that communication can take place as needed throughout the day rather than all at once at the end of the shift.
Team communication will be streamlined by using software that allows for easy scheduling, billing, and client interaction. Most crucially, a cloud-based EHR technology that permits shared access to client records across care team members allows for simple, yet safe, patient information sharing. As a result, each provider has access to the complete picture of a patient’s health and may make recommendations quickly without needing to consult other specialists.
Define individual roles and streamline work procedures
It’s critical to establish each provider’s function in a care team in order for it to be effective. This involves making recommendations for the patient and communicating with them on a regular basis. It’s especially vital to organize a patient engagement plan when working on a team with various doctors. If each provider they interact with checks in on them numerous times each week, asks identical questions, and makes similar recommendations, it can be overwhelming for patients. Delegating engagement duties to members of the team prevents communication with patients from becoming muddled, ensures that recommendations are followed, and makes them simple for patients.
It’s also crucial to distribute work to each provider throughout your team meetings. Patient interaction, drafting care plans, and arranging appointments are examples of these responsibilities. Assigning projects to unique providers ensures that nothing is repeated, saving time and resulting in a more productive team.
What proof does there exist for MDT according to the research?
- According to a comprehensive evaluation of MDTs in cancer services, all studies concluded that they boosted results. These included better treatment planning, more patient satisfaction and higher survival rates.
- In psychiatric services, enhanced teamwork leads to higher employee motivation.
- This has a positive relationship with the degree of choice available to those seeking help and their happiness with those options.
- By promoting collaboration among clinicians, MDTs can promote improved care coordination and quality.
- MDT sessions in cancer care can run up to 5 hours and comprise as many as 27 people.
- Only three specialists engaged on aggregate to the evaluation of everyone’s requirements.
- Primary care as a term that refers to the Hospital admissions for persons in high-risk populations: they have not decreased as a result of MDTs. In fact, hospital admissions have climbed somewhat.
MDTs appear to be helpful in fulfilling the demands of particular groups, according to research. They are highlighted as a fundamental desire of what successful integrated care looks like in SCIE’s Integration Logic Model. Enabling factors include a wide range of vocations and specialties, effective leadership and team dynamics, and supportive organizations.In Worcestershire, there are 14 Neighborhood Teams, each of which holds a monthly MDT meeting.
The following are some of the research’s key takeaways:
- Multidisciplinary teams have indeed been demonstrated to be an useful strategy for improving treatment outcomes by facilitating cooperation among experts.
- At the very least, successful collaboration necessitates the appointment of a manager or coordinator, the holding of frequents joint meetings, and the efficient exchange of electronic data.
- To operate effectively, teams do not necessarily need to be in the same location.
- Multidisciplinary collaboration may be addressed in a variety of ways.
- The MDT approach’s effectiveness is not assured: without strong organizational support, the impact might be detrimental rather than good.
Integrated care necessitates collaboration between experts and practitioners from many fields in order to meet the needs of individuals, their families, and their communities. Functioning together has been demonstrated to lead to a bad patient experience, a waste of resources, and in some circumstances, damage to individuals.
Teams that gather together appropriate professionals and practitioners are an excellent way to improve their work collaboration. These are frequently referred to as “MDTs,” although they are actually attempting to facilitate “inter” or “trans” collaboration amongst various “professionals” and practitioners. In many health facilities in the United States of America, the integrated teams are made up of populations ranging from 30-50,000 individuals, and each of these teams has its own MDT meeting where persons with the most complicated needs are discussed. This might involve the following:
- Mentally ill individuals
- Individuals in their eighties and nineties who have a variety of long-term illnesses.
- Individuals who are at a significant risk of being admitted and discharged from the hospital
In the United States of America, there is a government-run hospital. MDTs have certain similar characteristics, but they also have local variations that vary based on the team’s composition and the demographic the MDT supports. The following are common themes of public hospitals integrated teams and their MDTs according to the findings:
- A designated manager or practice leader who supervises and fosters the entire team’s efforts.
- A unique point of contact for all team members, including joint meetings to exchange concerns and ideas
- All team members’ interactions, evaluations, and interventions with an individual and their family are recorded in an electronic database.
- A ‘principal professional’ approach in which an identified team member coordinates care for people with complicated agency requirements.
Despite the fact that many of the teams are co-located, and while this is a goal, constraints such as distance and rent prices may make this challenging.
What are the goals that MDTs are supposed to accomplish?
No matter what demographic or need is being addressed, there is a common set of expectations for MDTs.
- MDTs will help experts and professionals from many fields better understand one other’s tasks and functions.
- MDTs will provide team members a common purpose and meaning, encouraging them to trust one another.
- MDTs will result in improved team trust and communication, as well as more holistically and person-centered therapy.
- Families and individuals will benefit from MDTs because they will avoid needless missteps and the unpleasantness that comes with them.
- Due to decreased redundancy, productivity increases, and preventative care methods, MDTs will result in more effective resource utilization.
- MDTs will minimize isolation among experts and practitioners, improving morale and lowering stress levels.
COVID-19 and the Multidisciplinary Team
If there’s one thing healthcare professionals have learned throughout the coronavirus pandemic, It’s because they necessitate a multidisciplinary team. To offer the greatest potential outcome for their patients, healthcare staff must also collaborate. The multidisciplinary approach to patient management and rehabilitation is critical when it comes to the numerous impairments that patients may face, as well as the rehabilitation components of these impairments.
COVID-19 has also demonstrated to health care providers how interconnected and vital the multidisciplinary team is. The corona virus has also shown that working together can assist healthcare providers achieve most of their rehabilitative objectives.
The Position of Speech-Language Pathologists in Covid-19 Management
The numerous neurological and problems that coronavirus patients experience at various stages highlight the need of speech-language pathologists in diagnosing and treating swallowing and communication problems. In the treatment of COVID-19 patients, speech and language pathologists are crucial.
Dysphagia or swallowing problems are a complication of ARDS caused by COVID-19. The respiratory system is harmed in ARDS, which might lead to problems with the respiratory-swallowing system. Food residue in the throat and aspiration into the airway are two symptoms of oropharyngeal dysphagia. In weak and immunocompromised older people, it is a risk factor for aspiration pneumonia. Ventilatory functions may deteriorate as a result of this. Patients with chronic Acute Respiratory Distress Syndrome (ARDS) may also need to be fed through a tube for respiratory support, which can cause laryngeal damage. It’s possible that this will impact your swallowing and voice. Dysphagia is a danger for a large number of extubated patients. Dysphagia after extubation has been associated to poor results, including:
- Elevated risk of contracting pneumonia
- Tubes for feeding are required.
- Malnutrition
- Lengthening of hospitalizations
- In-hospital mortality rate has increased.
The speech and language pathologist’s job is determined by the COVID-19 patients’ unique needs.
ICUs (Intensive Care Units) and ACUs (Acute Care Units)
- Dysphagia can be identified and diagnosed.
- Dysphagia is more common in severely unwell and acutely injured individuals who have contracted Covid-19.
- In patients who have been intubated for more than two days, a swallow examination is recommended before starting oral feeding.
- Johnson et al (2018) developed a dysphagia screening instrument that is often utilized by nursing personnel.
- Clinical bedside screenings, such as those performed by speech and language pathologists, are required, such as, Food and liquid swallowing trials, Medical history of the patient and an investigation of the oropharynx’s function and structure.
Units for Inpatient Rehabilitation
Patients are frequently sent to a hospitalization or transitional treatment facility centers once they are stable enough. The objective language and Speech pathologists treatment of dysphagia patients are to:
- Aspiration pneumonia should be eliminated or reduced.
- Optimize nutrition and hydration by dietary changes and behavioral interventions, for example. These therapies are dependent on a number of circumstances, including Comorbidities, Lung function, Age and the severity of the laryngeal trauma
Dietary changes
- For nutrition and hydration, enteral tube or nasogastric will feed intubated patients.
- To reduce the risk of aspiration, the speech and language pathologist evaluates the safety of oral feeding in collaboration with other members of the multidisciplinary team and recommends the least restricted food and liquid diet. (Physician, nutritionist, nurse, etc.).
- Dysphagia is linked to malnutrition and dehydration, as a result, collaboration between speech-language pathologists and dietitians is critical.
Reimbursement Training
Compensatory methods are recommended by speech and language pathologists to ensure that meals and beverages are consumed safely through the mouth. The following are some of these techniques:
- Variations in posture, such as: Head turn, Chin tuck and Sitting in a reclining position
These postural changes reduce the risk of aspiration by altering the bolus flow away from the laryngeal valve, its speed, and its direction.
During this phase, collaborations involving occupational therapists, physiotherapists, speech-language pathologists, and nurses are critical in determining the most optimal body alignment during mealtimes and monitoring the success of these compensatory tactics.
Behavioral adjustments, such as quitting smoking, and frequently Speech-language pathologists endorse it.
- To counteract physiological deficiencies, take small bites when eating.
- To promote aware and safe management of food bolus in the mouth, reduce surrounding distractions.
Exercises for Swallowing
Patients who use mechanical breathing neuromuscular weakening and reduced oropharyngeal sensitivity are possible symptoms. This could be the outcome of long-term intubation causing laryngeal injuries and not using oropharyngeal structures. When the patient’s breathing improves after extubation, To improve the strength and range of motion of the pharyngeal and laryngeal structures, the speech and language therapist may recommend swallowing exercises.
Management of a Tracheostomy
Illness that is critical Patients with Covid-19 who require prolonged mechanical breathing may benefit from a tracheostomy to help with ventilation weaning. Long lengths of intubation and delays in deciding whether or not to tracheostomise patients can result in:
- Atrophy of the muscles
- Vocal fold changes and hyolaryngeal motions
- Speech and swallowing may be compromised as a result of laryngeal trauma.
Aspiration has been linked to tracheostomy with and without artificial ventilation for the reasons stated above. Prior to starting an oral diet, a speech and language pathologist will assess swallowing in individuals with a tracheostomy.
Speech and language pathologists will assess whether or not a speaking valve is appropriate in consultation with the rehabilitation team. Patients with a speaking valve have a lower risk of aspiration, and their swallowing physiology and olfaction improve.
Oral Hygiene and Care
Bacterial colonization of the oropharynx is common in patients who have been intubated earlier. The following are some of the factors that contribute to this.
- Medication intake has increased.
- Reduced food or beverage intake through the mouth
- Dry mouth
- Old age
In Covid-19 patients, bacterial colonization in the oropharynx may enhance the risk of aspiration.
Patients are educated on oral hygiene and regular oral care by speech and language pathologists in collaboration with nursing staff and occupational therapists. This could include things like
- Brushing on a regular basis is recommended.
- Oral mucosa moisturization
- Preventing aspiration pneumonia by managing oral secretions
Delirium Screening
Patients with the Coronavirus may get perplexed, disoriented, and delirious. This could be due to a number of factors.
- Respiratory treatment that is too intrusive for a long time
- administering a sedative drug
- In the wards, there is a lot of social isolation.
During their meetings with patients, to reduce the risk of delirium, speech and language pathologists can help. The steps taken are:
- Orienting the patient to the current moment, location, personnel, and circumstances
Involve the individuals in exercises that stimulate the brain.
Units for outpatient rehabilitation
Speech and language pathologists may continue to use dysphagia intervention tactics in various outpatient settings, such as clinics, private practice, and home-based therapy.
- Oral dietary changes
- Strategies for compensation
- Exercises for swallowing
- Long-term dysphagia and respiratory distress disorders that affect voice and cognition can also be treated.
Enhancement of Speech Intelligibility
Patients who have a tracheostomy can be taught to swallow and speak by speech and language pathologists.
- Occluding the tracheostomy digitally
- Using a one-way communication valve: In individuals with tracheostomies, speech therapy using a one-way valve improves speech intelligibility and quality of life.
Voice Rehabilitation
Voice hoarseness and regular throat cleansing are symptoms of post-intubation dysphonia. This is common in people who have been on endotracheal intubation for a long time. Following extubation, the vocal structures begin to physically heal and the voice may improve. In patients with chronic dysphonia, speech and language pathologists can assess vocal parameters and teach patients about vocal hygiene and strategies to improve voice projection and quality.
Neurocognitive Management
ARDS survivors have been documented to exhibit cognitive abnormalities. These flaws encompass:
- Impaired verbal fluency
- Global intellectual deterioration
- Memory impairment
- Decreased concentration
- A lack of executive function
These deficiencies can have an impact on a person’s overall impairment and quality of life.
To provide adequate treatments, Psychologists and cognitive behavioral therapists can collaborate with speech and language pathologists. These include
- Screening for cognitive impairment
- In-depth evaluations of each cognitive domain
- Offering cognitive training exercises that are appropriate
Occupational Therapists’ Contribution to Covid-19 Rehabilitation
Occupational therapists assist individuals with physical disabilities, cognitive, emotional, or developmental disabilities to provide remedial and restorative therapies and rehabilitation.
Acute Care
Occupational therapists can practice in a variety of settings, including critical care or acute care units. These healthcare workers have a particular set of skills as well as a special focus. Their treatment approach is comprehensive, taking into account the person-occupation-environment relationship, in addition to their assessment process know-how, may give the critically ill patient with numerous benefits and favorable outcomes. In hospital settings, both remedial and restorative care can be provided by occupational therapists..
According to the needs of the patient and the degree of the Covid-19 virus, Interventions in the areas listed below may be necessary:
- Delirium prevention, identification, and monitoring
- Physical and cognitive functioning deficits are both assessed and managed.
- Applying pressure-relief concepts modify and improve bed and seating placement.
- Maximizing respiratory function through positioning
- Mobility in the bed
- To stimulate early mobilization, assess and manage daily living activities. Grooming hair, cleaning teeth, and grasping and sipping from a mug are only a few examples.
- Assistive equipment for ADLs, communication, seating, and mobility are assessed and provided as needed.
- To improve social engagement, communication management is used.
- Examine the patient’s mental health and suggest emotional coping skills.
- Stimulation of the senses
- Conservation of energy
Post-Acute Care
Occupational therapists can be quite helpful during the post-acute phase of Covid-19 therapy.
The following are some of the broad management principles that apply to a variety of situations:
- Reevaluate and treat cognitive changes to help you achieve functional independence.
- Discharge from the hospital or rehabilitation center preparation and planning. This covers things like patient monitoring inspections and caregiver assistance.
- When preparing for discharge, take into account social determinants of health (such income).
- Daily life activities are reassessed and managed. Adaptive methods such as assistance gadgets and energy saving are examples of this.
- Assess and take into account the patients’ and caregivers’ mental health and psychosocial needs.
Collaboration between occupational therapy andphysiotherapy
The management of Coronavirus patients has benefited greatly from collaborations between occupational therapists and physiotherapists. Because the patients are initially weak and have little endurance, physiotherapists and occupational therapists frequently collaborate and see the patients at the same time. Occupational therapists and physiotherapists can work collaboratively in Covid-19 patients to address mobility and daily living activities.
In rehabilitation facilities where a speech and language pathologist is not always accessible, By urging patients to drink a few sips of water, occupational therapists and physiotherapists can help with patient care and swallowing exercises, for example. Frequently, the treatment and rehabilitation objectives are intertwined, and via partnership in the care of Covid-19 patients, the Occupational therapists and physiotherapists are in a unique position to achieve the goals of independence, respiratory rehabilitation, and function maintenance. Whenever patients have gained sufficient strength, therapy sessions can be divided and particular rehabilitation goals can be addressed. Patients should be able to carry out fundamental everyday tasks as soon as feasible after being discharged, if at all possible. Physiotherapists and occupational therapists play a crucial role in this.
Dietitians’ Covid-19’s Role in Rehabilitation
Dietitians are properly qualified nutritional professionals who specialize in supporting the nutritional and hydration requirements of individuals who are severely or chronically unwell.
Nutrition experts are in the greatest position to monitor Covid-19 patients’ nutritional condition at all levels of care.
Acute Care
The intensive care unit will sedate and mechanically ventilate many dangerously ill Covid-19 patients. Nutrition, hydration, and medications are delivered to these individuals by feeding tubes. The feeding tubes provide these individuals with the essential proteins and calories. The dietitian’s job is to make sure the patient gets the best nutrition and hydration possible. A dietician will evaluate a patient with Covid-19’s dietary needs by taking into account a variety of criteria:
- Age and gender of the patient
- Medical problems that are causing the problem
Poor nutrition or changes in eating patterns can occur in chronically unwell people. There is a loss of smell and taste in Covid-19 sufferers. This may have caused the patient to lose his or her appetite before to admission, and the patient may already be malnourished. It’s possible that this will continue following a catastrophic sickness. This could have a significant impact on the patient’s recovery and rehabilitation.
In addition, certain sedatives contain calories. When prescribing feeding regimens for a patient; this must be taken into account, as overfeeding can be hazardous to a critically ill patient in the acute phase of the illness. Propofol will be used to sedate a large number of severely unwell patients. This is a lipid solution, which adds up to a lot of calories when infused continually. Other medications, such as prokinetics, are used to help the stomach contents empty more quickly. This is particularly critical if the patient is prone to infections. Patients may also require quantity limitations to control respiratory issues, as well as more concentrated energy-dense feeds, which can induce gastrointestinal discomfort. Nutrition experts are essential in keeping track of all of these variables and avoiding any potential problems.
Post-Acute Care
Even after being discharged from the hospital following a Covid-19 infection, a patient may require the assistance of a dietician. Dietitians have a key role in Covid-19 patients’ post-acute recovery. The risk of problems can be decreased, and the patient’s recovery period can be shortened, if correct dietary guidelines are followed. Malnutrition is a concern for patients recovering from a severe Covid-19 infection. They will almost certainly have lost muscle mass throughout their hospital stay due to severe sedation and inactivity. Dietitians can assist these patients by prescribing nutrient-dense, fortified foods or specialty nutrition supplements to aid in their rehabilitation and the regaining of weight and muscle mass lost during their illness.
The Physiotherapist’s Contribution in COVID-19
Patients hospitalized with suspected or confirmed COVID-19 will very certainly be managed by physiotherapists who work in primary care settings. Physiotherapists and other professionals are vulnerable to infectious illness transmission due to their close contact with patients. Physiotherapists are frequently first-contact practitioners, which mean they might take responsibility for early detection of infectious illness and/or workload management in primary care settings. Physiotherapists and other health professionals must thus be acquainted with COVID-19 and how to avoid its spread, as well as how they may participate in workforce planning. They should use their professional judgment to decide when, when, and how to give care, keeping in mind that this is not necessarily the best setting for everyone concerned.At the same time, we must remember that our profession is critical to the health of our community, and that there are individuals in our communities whose health may be adversely affected by care interruptions.
The Multidisciplinary Team Approach in oncology
In oncology, a multidisciplinary team is described as collaboration among a number of cancer-care specialists with the overarching goal of improving treatment quality and patient care. Neck and head cancer is made up of a variety of illnesses that are biologically unique and require various treatments. The psychologically and physically consequences of cancer, as well as patient symptoms and treatment side effects, will vary depending on the disease site and treatment approach. In contrast to the previous notion of a worldwide therapy given by a single physician, combining the efforts of many experts is considered to improve patient care.
In the mid-1980s, it was discovered that combining chemotherapy with radiation or surgery improved survival; in oncology, the interdisciplinary approach became prominent. Meanwhile, with the development of new treatment procedures, organ preservation strategies in HNC began to emerge. The MDT started out as a supervised panel that assessed all new people with cancer and concurred on a treatment plan devised by radiation and medical oncologists, as well as surgical doctors, on the basis of their clinical experience and information.
When MDT representatives realized that this strategy was really enhancing patient care, they decided to add other specialties focusing on supportive treatments to the MDTs. By preventing and minimizing treatment side effects, the addition of the latter group of specialists improved cancer care quality, which increased patient adherence and compliance to treatments. Oncological functional unit’s establishment, malignancies that are particular to a disease location, with a focus on cancer patient treatment and care, was a natural progression of this strategy.
These units incorporate a multidisciplinary panel that includes all agencies involved in the treatment of a patient, with the goal of shortening time to diagnosis and/or therapy initiation by facilitating intervals and interactions between the various experts.
The HNC Specialized Clinical Nurse’s Role
Because of its location, HNC is frequently associated with a variety of functional and physical complications, necessitating extensive bio-psycho-social care. It will be critical to provide patients with full assistance from the moment they are diagnosed in order to finish the treatment plan. In this illness, the function of the expert clinical nurse, as an important member of the MDT, aim to provide patients with assistance throughout the screening and therapeutic procedures, which encompasses not just nurse interventions but also functional case management, such as treatment management and scheduling..
The nurse will function as a facilitator and coordinator for all of the MDT’s expertise, integrating healthcare processes in collaboration with other cancer care providers and arranging their actions in care plans. From the patient’s and family’s perspective, All through the patient encounter, the nurse is the bedrock that maintains care continuity, follow-up is included.
The nurse will do a thorough examination of the patient and family at the time of diagnosis. It is critical to create a positive connection with the patient and his or her family in order to Include them in the decision-making process, and educate them on how to avoid and manage treatment toxicity, as well as how to spot new symptoms. This connection is critical for ensuring patient adherence and treatment compliance, as well as maximizing healthcare resources.
As part of the HNC MDT, the nurse specialist’s responsibility is divided into three areas:
Case management
In this complicated disease, case management is defined as a systematic attempt to coordinate patient and family treatment. The major aim from a methodological standpoint is to obtain better care results more effectively, since this will allow for better control of professional resources, which will have an influence on health expenses. The case management approach is used by the nurse in the context of a specific process or condition, in these instance HNC patients in a hospital setting. During the entire process of patient care, one of the nurse’s goals is to collaborate with and coordinate all of the experts that make up the MDT.
From diagnosis through follow-up, the nurse is the cornerstone for the patient and family, and she plays an important supportive role until the acute toxicity is resolved.
During the diagnosis and treatment planning process, the nurse ensures that all scheduled appointments and essential diagnostic evaluations are completed on time to minimize needless delays in treatment initiation. This is especially essential for individuals who are receiving multimodal therapy simultaneously or sequentially. The nurse will not only guarantee that therapies are scheduled appropriately, but will also assist in their adaptation at each stage depending on the specifications and demands of each patient.
One of the nurse specialist’s most essential responsibilities is to provide immediate support to patients and families via a direct link during the day. This will enable the nurse to address patient questions or concerns, assist in the management of side effects and symptoms, and screen for potentially serious issues that require immediate treatment and/or referral to the emergency room. Furthermore, it enables treating physicians to be informed of any important event, symptom, or toxicity at all times, allowing them to arrange visits and/or change therapies as needed. Nursing care must be included into the formulation and execution of clinical guidelines, according to the nurse.
Operational role
To prevent delays, the nurse makes sure that patient referrals from general care or local specialists are arranged as soon as possible, and she connects patients who require multimodality therapy with doctors from several departments. The nurse schedules an appointment with the new patient and family/caregivers once the HNC interdisciplinary committee has approved a treatment choice. A complete evaluation of the patient’s medical and psychosocial state, as well as support needs, is done during this first appointment. The nurse provides information about the therapy, including the strategy and logistics, as well as an explanation of the toxicity and the resolution of any queries or issues that may arise. This visit is crucial in consolidating the information provided by the expert physician before.
Aside from doing a complete and customized evaluation, extra attention is paid to detecting any potential changes that might obstruct the typical therapy dynamics. This is very important for HNC sufferers. Assessment of nutritional status, swallowing and phonation, dental evaluation, psychological support, rehabilitation, toxic habit evaluation, oncogeriatrics, and palliative care are all examples of circuits that are triggered to help patients based on their requirements. The nursing documentation for patient evaluation is based on a concept based on Marjory Gordon’s Functional Health Patterns.
Medical assistance
A significant duty of the HNC specialist clinical nurse is to give clinical support. The following areas of nursing care are prioritized at HNC:
- After the effects of the diagnoses as well as during treatments, offer emotional support to patients and their families.
- Patients and family members get health education on the prevention, early diagnosis, and management of symptoms and side effects, as well as methods to increase their autonomy.
- Various fields of healthcare collaborations
- Gastrostomies and Feeding tubes management
- Tracheostomies management
- Management of treatment-induced dermatitis, post-surgical treatments, and toxicity
Dental Care for HNC Patients
Dental care is critical for HNC patients and must be included at every step of the oncologic process. This procedure includes several stages, each with its own set of challenges. It’s critical to keep track of the potential problems that might arise in the oral cavity as a result of chemotherapy and radiation. Because of the potential of problems, any dental operation should be avoided during chemotherapy cycles. Chemotherapy-induced thrombocytopenia and neutropenia can cause bleeding as well as fungal, bacterial, and viral infections. Chemotherapy patients, particularly those undergoing methotrexate, cyclophosphamide, cisplatin, and fluorouracil, might develop mucositis, which can have a negative impact on oral cavity health. Patients with HNC who are having oncologic therapy must pay special attention to their dental health. If at all feasible, any dental therapy should be preventative, as any dental treatment following oncologic therapies would be less effective.
Methodology
Selection of Cases
The author decided to do a case study comparing four COVID 19 hospitals in the United States of America. Since they engage with inherent relationships rather than merely frequency or incidences, that need to be translated, comparative case studies are particularly well adapted to answering explanatory research concerns. In this research, the matter is about the analytical unit, which is the government hospital. The author concentrated on COVID 19 hospitals since the changing disease history and symptoms of COVID necessitate ongoing, multidisciplinary treatment. The author looked at multidisciplinary teams from four government-accredited COVID 19 hospitals in New York City, which provided similar treatments and operated in identical legal circumstances.
All four COVID 19 treatment facilities were chosen to maximize the chances of identifying variations in work organization. Despite significant disparities in financing arrangements, all healthcare facilities provided patients with the same illness with equivalent ambulatory and inpatient treatments. These services were particularly assessed to ensure that the core processes and all required activities were consistent among hospitals.
The fundamental processes must be comparable for the sake of this research, but the work organizations should be different. Disparities in legal framework and organizational scale can also be seen. Two of the institutions were completely managed affiliates of a public hospital, whereas the other two were independently operated. As a result, the institutional size of the two branches (i.e., 5 and 25) was significantly less than that of the independent institutions (i.e., 55 and 135).
Despite the fact that large organizations are frequently linked with effective work organizations, previous research and the businesses that took part in this study show that workplace structure is not necessarily determined by size. To ensure that the cases remain anonymous, no more identifiable information is provided.
Data Collection
Personal interviews with healthcare professionals (n = 35) on spot were the primary source of data used in the study, which were performed throughout March 2020 and June 2021. The relevant government agency in the United States of America granted ethical approval. Subject interview questions were a good way to get information. To obtain the desired details, individualized, open-ended, relevant interview questions were required. The interviews, which were conducted utilizing case-related resources such as inspection reports, were conducted using a subject guide, PowerPoint presentation, and patient pamphlets, to guarantee consistency in our data gathering.
The reconstruction of the treatment process from the patient’s perspective was a recurring subject throughout the topic guide, allowing researchers to learn more about team composition, working relationships, and therapeutic connections. There were 3 main categories in the interview guide.
- the function of the respondent in the institution
- teamwork between members of the same healthcare team
- cooperation with other departments’ and team of healthcare providers
Each domain’s interview began with the identical introductory questions.
- What are your responsibilities at the healthcare institution
- With whom do you build a team
- What does it look like when you collaborate with different teams and departments?
In order to interpret their jargon and dive deeper into the intricacies of the work organization, additional questions were asked based on the substance of the interviewee’s responses, Workplace connections, team structure, and therapeutic ties a total of 15 nursing care providers were questioned, 12 paramedical care providers and 5 healthcare professionals with the amount of interviews varying per hospital. The number of interviews was larger (n = 18) Since the number of interviews required to accurately identify the work organization was being examined as part of the data collection and analysis procedures in the first hospital we looked at.
Ten nursing care providers, six paramedical care providers and Two medical care providers, and were interviewed in the first hospital. However, it was quickly apparent that considerably fewer interviews were required. Six interviews were performed at the second hospital. Two nursing care providers, two paramedical care providers and Two medical care providers, and were interviewed. One nursing care provider, two paramedical care providers and One medical care provider, (n = 4) were interviewed at the third hospital. In the fourth hospital, three care providers (medical, paramedical, and nursing) were questioned.
Data Analysis
To structure the research and explore the genuine kinds of work organization inside the Covid 19 health facilities, the author employed the theoretical framework. The goal of the analytical method is to figure out which sort of work organization each situation requires. Despite the fact that the work organizations of the hospitals were not explained before to the interviews, they quickly appeared in the topic interviews through immediate interpretations and follow-up queries. In a sense, the data gathering and analysis processes collided, yet this isn’t an issue for two main reasons. Firstly, the interviews, as well as the contemporaneous interpretation of data and categorization of the instances, were driven by a prior theoretical knowledge about probable work organization variations.
The opinions of key informants on how tasks were split and organized into organizational units were matched to the appropriate work organization, the makeup of the team, relations of working and therapeutic partnerships, with a particular focus on any departures from classic mental definitions. Second, in order to eliminate subjectivity, inter-researcher triangulation was set up. To minimize mistakes and misunderstandings, the initial author’s categorization was extensively examined.
Finally, so that we may answer our research question, the 4 covid 19 healthcare centers hospitals had to be distinguished by different forms of work organization. Each instance had a unique work organization, resulting in a wide range of results.
Results
On the grounds of their operational organograms, the four covid 19 hospitals looked to be identical in terms of work organization at first glance. Moreover, because organograms are typically poor representations of what happens inside an organization, the work organization was found to differ significantly in actuality.
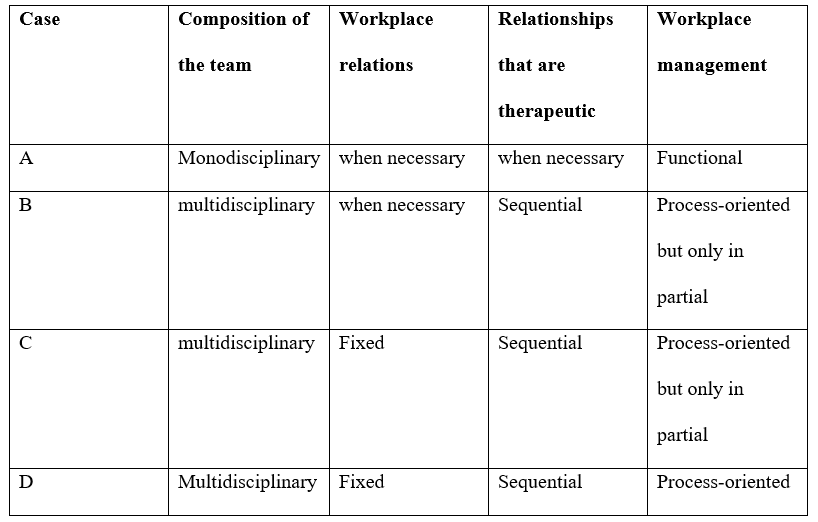
The first example involved COVID 19 health centers, which had a well-functioning work organization. The overall goal of providing patient care was broken down into individual tasks, they were then divided into functional areas and structured into organizational units. Contrary to the hospital’s claim of multidisciplinary teams, nursing departments, paramedical and the monodisciplinary medical, teams were the organizational units to which responsibilities were given. Nursing care providers maintained stable working connections with other nursing care providers, resulting in monodisciplinary teams.
The second example was the Covid 19 health facility, which included a partial version of process-oriented work organization. The composite job was broken down into individual tasks, which were then organized cross-functionally into temporary interdisciplinary organizational units. To put it another way, an ad hoc (when necessary) multidisciplinary team was formed every time a patient enrolled at the covid 19 health centers until the end of an unplanned care period.
Since duties were assigned to organizational units that corresponded to a defined phase of the healthcare setting rather than the healthcare system as a whole, this type of process-oriented work organization was termed incomplete. The MD stayed the same throughout all care phases, and therefore throughout the whole care process, but paramedical and nursing healthcare professionals were allocated ad hoc to service a single patient for the duration of a certain care phase, and, more crucially, they changed between care stages. This indicates that clinicians did not have established working connections with one another.
A limited type of process-oriented work organization was also present in the third example. Per care phase, the composite job was split into different tasks that were cross-functionally grouped into multidisciplinary organizational units. The distinction between the first and second cases is that fixed multidisciplinary teams were created rather than ad hoc multidisciplinary teams related to specific, specified care plans. Short- and long-term ambulatory rehabilitation, hospitalized rehabilitation, hospitalized medical intervention, and chronic hospitalization are among the treatment options. As a result, in the framework of the care program, care professionals from many fields collaborated on a regular, consistent basis.
Work was organized in a process-oriented manner in the fourth example. Per care process, the composite job was split into separate tasks that were cross-functionally grouped into multidisciplinary organizational units.MS patients, in particular, would always be treated by the same multidisciplinary care team.
Using a comparative case study, the paper demonstrates how a systemic view through the notion of work organization uncovers the many organizational configurations that may underpin ostensibly multidisciplinary teams. Depending on the sort of underlying work organization, the actual makeup of multidisciplinary teams, as well as the related working and therapeutic interactions, will differ. To be more specific, the more process-oriented the work organization, the more stable and constant the working connections and therapeutic looked to be.
Discussions
Conclusion
A multidisciplinary team environment benefits everyone. Patient-centered, efficient, and cost-effective treatment is provided, and patient and professional satisfaction is higher. In addition, Multidisciplinary teams have been shown to have beneficial results for persons and their families, as well as enhanced work satisfaction for experts and practitioners, according to studies.This is not assured, and MDTs can have no influence or, in some circumstances, a detrimental impact if they are not adequately organized.
References
Science Organization UK. (2021). Multidisciplinary teams – Activities to achieve integrated care. Social Care Institute for Excellence (SCIE). Retrieved 7 July 2021, from https://www.scie.org.uk/integrated-care/research-practice/activities/multidisciplinary-teams.