The Impact of Insufficient Registered Nurses on Patient Care in Acute Care Hospitals in the UK
Number of words: 8723
INTRODUCTION
This study intends to explore the impact of insufficient registered nurses on patient care in acute care hospitals in the UK. Notably, there has been a shortage of registered nurses, which has been associated with various negative implication in the delivery of care. My motivation to study this topic was derived from the experience gained in placement. During the day shift they were short of staff and it was only two registered nurses that were on duty that day with 24 bed in the ward. Notably, the nurses were struggling to provide quality care to patient as 12 patients were allocated per a registered nurse. The two nurses overworked that day, a factor that made them unhappy about the working environment. Even though a nurse assistant and I assisted in the care given to patients, it was not enough as we were limited to some tasks. As such, this study intends to explore the effects of the shortage of registered nurses and the different strategies that can be used to tackle this problem among the healthcare settings in order to improve the quality of care we deliver to patient.
The purpose of the study is to explore the impact of insufficient registered nurses on patient care in acute care hospitals in the UK. It also ensures that the NHS is aware of the need for changes in the healthcare sector, particularly in regard to the number of nurses to promote the delivery of services. As such, this study creates awareness and a possible avenue of solving registered nurse shortages, especially within acute hospitals.
The largest group of professionals in the global healthcare system are registered nurses (RN). (Monahan, 2015). Worldwide, there are approximately 19.3million nurses (Flinkman et al., 2013). Nursing vacancies are increasing exponentially in the UK. The English National Health Service (NHS) nursing workforce had 41,000 RN vacancies in October 2018, alongside an 11.8% vacancy rate, which was 9% higher than in 2017 (NHS Improvement, 2018).
Insufficient RN staffing has been suggested as a strong causative factor for preventable deaths and deficiencies in English hospital-care (Francis, 2013; Keogh, 2013). Many individuals have researched on the impact of nursing on patient care, but very few have concentrated on the shortage that has derailed healthcare provision within the United Kingdom. The topic becomes a matter of interest globally since there is an urge to achieve universal health(Aiken et al., 2007). In NHS hospitals, there is a bigdissimilarity of patient-to-RN ratios, thus meaning that one RN cares for a large number of patients, and this has been linked to higher in-hospital mortality-rate (MR) (Aiken et al., 2014; Griffiths et al., 2016; Rafferty et al., 2007). Empirical evidence from many studies worldwide including the UK suggest that low RN-staffing-levels (RN-SLs) are associated with mortality (Aiken et al., 2012;Aiken et al., 2014; Griffiths et al., 2016). Whereas there are fewer studies that associate low RN-SLs with missed care or low patient-care quality (Aiken, Clarke and Sloane, 2002; Aiken et al., 2012; Sochalski, 2004).
Insufficient nurse registration has derailed issuance of professional care to acute patients in most hospitals worldwide. Low nurse-patient ratio indicates that something has to be done to promote provision of quality healthcare services. In the United Kingdom, there are over 300000 registered nurses who offer the required care to patients, especially within acute hospitals. Aged patients need more patient care than younger generations within the United Kingdom. In the elderly wards, nurses are required to provide the required support for such individuals to heal, unfortunately, the number of nurse availed in such wards is not enough to suffice the need(Cardona-Morrell, 2016; Petersen, Antonsen and Rasmussen. 2016). The eventual impact is that the quality of care is compromised, which sometimes leads to deaths in various hospitals within the United Kingdom (Aiken et al., 2007). The government of the United Kingdom and all stakeholders in the healthcare sector should team in a bid to find a sustainable solution.
Research also suggests that low RN-SLs, low nursing-care quality and eroding skills-mix in hospitals are associated with adverse-outcomes, e.g. falls, mortality, hospital re-admissions, pneumonia, infections, medication-errors and pressure ulcers. (Ausserhofer et al., 2013; Griffith et al., 2016; Kane et al., 2007; Schubert et al., 2008). Whereas increasing RN-SLs was associated with lower adverse-outcome rates (Griffith et al., 2016; Kane et al., 2007). Initially, NHS workforce initiatives blamed the hospital-care and quality deficiencies on “uncaring nurses” (Smith, 2012; Aiken et al., 2014a). In 2018, a House of Commons Health and Social Care Select committee on the how little attention has been given to nurses who are overworked and unable to cope with workload whilst providing quality care (House of Commons Health Committee, 2018). Likewise, the English National Advisory Group on patient-safety stated that NHS staff shouldn’t be held responsible for the declining hospital-quality, but more emphasis on inadequate RN-SLs should be made (National Advisory Board on the Safety of Patients in England, 2013).
Reasons for nursing shortage include supply and demand problems, along with healthcare structure alterations and the growing aging-population. Likewise, a decrease in RN training intakes, and difficulties in RN-employment and retention are responsible for UK RN-shortages. The issues with the demand and supply for NHS staff have been highlighted by the Chief Executive of NHS Improvement, who stated that a 5-years strategy has been put in place, however, before then, NHS nursing-shortages would continue (Collins, 2018; House of Commons Health Committee, 2018). Likewise, the amount of nursing university-graduates has not met the high demand for nursing care (Dunn, 2014).
The need to adequately cover all areas within a population prompts the government of the United Kingdom to work hard in a bid to ensure that healthcare services are provided efficiently(Griffiths et al., 2018c; Recio-Saucedo et al., 2018). Patient care and health provision should align with the number of practitioners that are available in the field. In most cases, there are more patients than nurses in the healthcare sector, a factor that has led to poor service provision. The gap between patients and nurses should be reduced to enhance proper efficiency. In essence the research seeks to answer the question “what is the impact of an insufficient registered nurse on patient care in acute care hospital within the United Kingdom?” The research will apply strategic approaches to acquire necessary materials to answer the research question.
There is a decline in the number of nursing-university-students (24%) expected to graduate in the normal university allocated-timeframe. (Aiken et al., Buchan et al., 2019; Department of Health and Human Services, 2016; 2017). New NHS workforce initiatives and British policy-schemes to tackle nursing-shortages and maintain safe and quality hospital-care includes introducing nursing-degree apprenticeships, and nursing associates (NAs) (House of Commons Health Committee, 2018). Likewise, social care staff are also being enrolled into the NA-scheme. (NHS Digital., 2018).These staff are all markedly less-qualified than RNs. Thus, this might not be the best solution to improve hospital workforce because they are less skilled and trained than RNs. Thus, this erodes nursing skill-mix, which research associates with increased MR and decreased patient-outcomes, and these factors are also linked to inadequate RN-SLs (Aiken et al., 2017; Dall’Ora et al., 2019).
Likewise, this opposes the 2010 Prime Minister’s Commission on the Future of English Nursing and Midwifery recommendation that states that every nursing education should occur only in university due to empirical evidence, which suggests that significantly high hospital patient-outcomes are associated with bachelor-prepared nurses (Aiken et al., 2003; Aiken et al., 2014; Yakusheva, Lindrooth and Weiss et al.,2014).
Although, it can be argued that more less-skilled staff can potentially improve nursing-care quality and adverse-outcomes e.g. decrease falls. (Alvarez et al., 2011; Bae et al., 2015; Xue et al., 2012). Nonetheless, some research suggests otherwise. (Bae et al., 2014, Wu and Lee, 2006) However, increased employment of such staffing can increase hospital salary costs and pay rates (Hurts and Smith, 2011).
Similarly, less-trained temporary-staff (agency- or hospital-bank-staff) can potentially mean team communication and continuousness care disturbances, and decreased acquaintance with unit practices, hence, impairing quality and safe care (Aiken et al., 2007). Likewise, Brexit, immigration policy alterations alongside reformed language testing requirements for international-nurses caused a drop in the influx of EU health-professionals, which has consequently increased non-EU nurses’ employment (Buchan et al., 2019).
The magnet hospital model has emerged lately to provide a framework for practice and future research in nursing and healthcare(Dall’Ora et al., 2019; Griffith et al., 2018; Griffith et al., 2019; West et al., 2014). By the year 2011, over 6.61% of hospitals that are registered had acquired a magnet recognition, which has been helpful in promoting patient care in cute hospitals, especially within the United Kingdom. The model serves as a roadmap for all organizations in the healthcare sector that want to achieve magnet recognition. Also it values nurse recognition and appraisal as a way of enhancing retention within healthcare providing institutions.
RESEARCH QUESTION and AIM
Following the introduction, the research question and aim of this review focuses on analysing the impacts of low RN-SLs on three main themes:
- patient-to-staff ratio,
- missed care, and
- mortality in in UK acute care settings i.e. hospitals
The following was performed to achieve the aims:
- Increase familiarity with published literature
- Produce an efficient and appropriate search methodology
- Establish a thorough data-extraction form
- Complete a systematic and comparative review of chosen literature
MATERIALS AND METHODS
A systematic review of the literature was done to explore and find main research primary papers using a thorough method (Ganeshkumar and Gopalakrishnan, 2013).
Research Question
At the beginning of the dissertation, current articles and systematic reviews were sourced to become conversant and familiar with the chosen topic on RN-staffing levels impacts on hospital care.
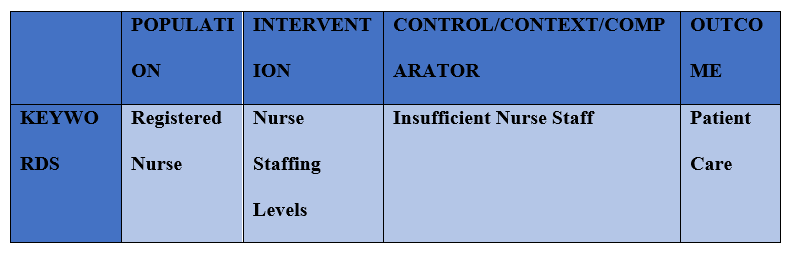
This helped to produce a defined topic and aim, and create an applicable PICO (population, intervention, control and outcomes) analysis (see, Table 1 below). The PICO analysis aided in comprehensively investigating the topic, and initiating the development of the search strategy by increasing suggestions for the search terms used in databases.
Table 1. PICO Analysis. The initial procedure performed to generate an appropriate research question and an organised search strategy.
Search Strategy
Databases
An electronic systematically literature search was performed on the following databases: BRITISH INDEX, CINAHL, PUBMED, GOOGLE SCHOLAR, MEDLINE, and ROYAL COLLEGE OF NURSING. These databases are large databases that encompass a huge amount of primary research articles concerning healthcare and medical research.
Search Terms
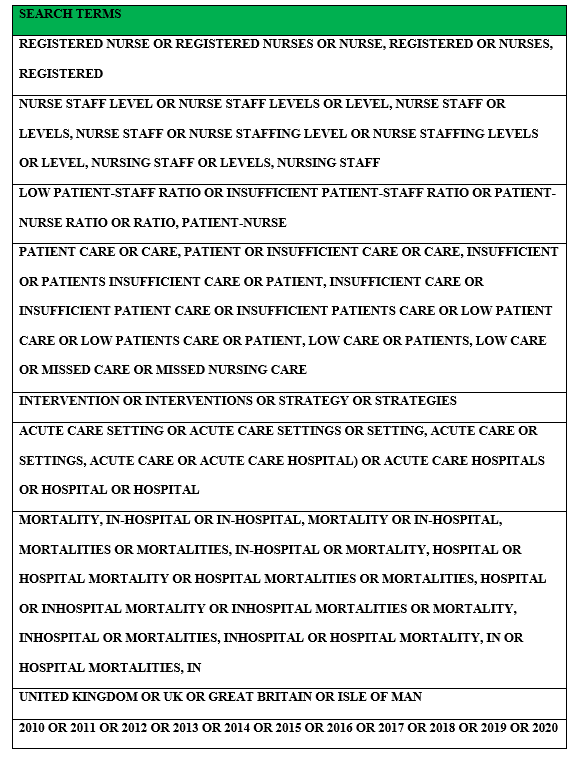
The important keywords and medical subject headings (MeSH) terms include *registered nurse*, *low nurse staffing level(s)*, *patient-to-staff ratio*, *patient care*, *missed care*,*intervention(s)*, *low quality of care*, *mortality*, *acute care setting(s)*, *hospital*, *in-hospital mortality* *United Kingdom* (see Table 2, below).
Table 2. Search Terms. The main search terms used for database search.
Hand-Searching
Hand-searching was done using Google search, checking reference lists of articles and reviews, and predominantly, Google Scholar in order to ensure thorough search on the topic is done. This secondary search helped to provide more articles for inclusion in the final analysis (see PRISMA flow-chart [see, Figure 1]).
Inclusion and Exclusion Criteria
Inclusion Criteria
- Primary studies (e.g. qualitative, observational, cross-sectional studies)
- Primary studies performed in the UK
- Primary studies between years 2009-2020
- Primary studies that focus on RN-staffing levels impacts and the three theme (all in a paper or in different papers)
- Adults and elderly patients
- Primary papers on RN-staffing levels impacts in hospitals
Exclusion Criteria
- Secondary papers e.g. articles, discussion papers and reviews
- Studies that include the questionnaire method
- Related/Relevant studies outside the UK
- Related/Relevant studies on neonates or children
- Papers not in English
- Studies later than year 2009
Study selection
So as not to deviate from the aims of the review and to focus on studies performed in the UK between 2009-2020, only few results were generated in the database search. I was tempted to broaden my search to Europe or worldwide, however, I realised that this would jeopardise the main aim of this study to find correlations and solutions associated with low RN-staffing levels, which is a major issue for the NHS.
Data Extraction
Full texts of papers were accessed post title and abstract review. A data extracted form was developed using Microsoft Word. Data extracted included: author, study design, method used (tools), study population, primary outcomes and secondary outcomes (associated with this review’s primary and secondary aims), conclusions, comparisons to other studies and future research.
Included studies
The number of articles sourced from each database is present in Table 3.
The PRISMA flow chart outlines the article review process in Figure 1.
Table 3. Database and Hand Searches. The Results of both searches for articles.
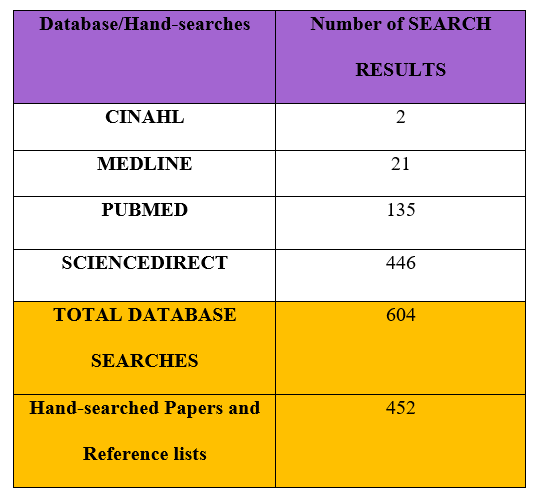
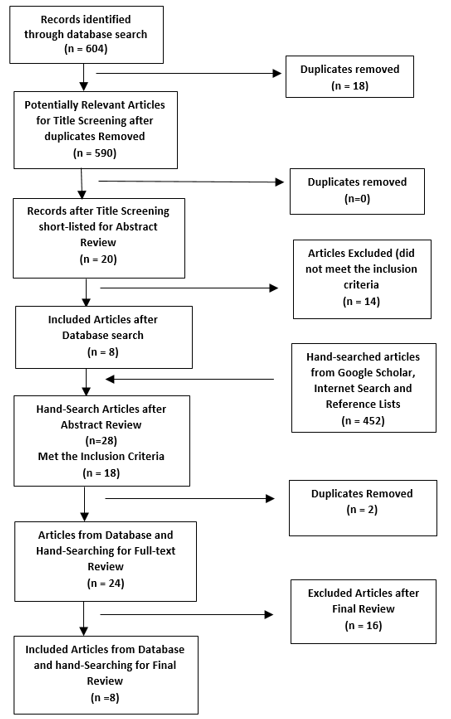
Figure 1. The PRISMA flow chart of Included Articles.
Avoiding Bias
The inclusion and exclusion criteria were strictly-adhered to because the topic was chosen out of personal interest.
Quality of Studies
The Cochrane Risk Bias Tool is a common guide used to measure the quality of included studies (Handbook-5-1.cochrane.org, 2020). However, this was not assessed due to time-constraints and nature of studies. However, in the discussion section, papers were comprehensively criticised for study procedures, tools and bias.
LITERATURE REVIEW
THEME 1: Patient-to-staff ratio
A major focus of this review and a key question in the healthcare setting worldwide is ‘what is the right threshold or limit of patients per clinical staff?’ This topic is very important because healthcare staff workload determines the nursing-care quality given to each patient.
Three main studies covered this theme (Bridges et al., 2019; Smith et al., 2010; Unison, 2017).
An observational research was used as the data-collection method in Bridges et al., (2019) to study RN and healthcare assistant (HCA) staffing levels, and daytime quantity- and quality-of-care for 270 adults in six wards at two English NHS hospitals. The participants in the study were aged between 18 and 101 years, with an average age of 82. The number of nurses who got involved during the study is 44. There was that there was an average of 6.9 patients-per-RNs found a three-fold increase in the odds of a negative-interaction occurred when one RN took care of ≥8 patients, which is high compared to reference staffing category of >6 and <8 patient-per-RN. Although, no such association was found with HCA-staffing. In cases of high HCA-staffing (<7 patients-per-HCA) and high RN-staffing (≤6 patients-per-RN) or medium (>6 to <8), rates of negative interactions were low. But high HCA-staffing and low RN-staffing (≥ patients-per-RN), high rates of negative-interactions occurred.
Likewise, in a retrospective observational study (Smith et al., 2010) performed in an acute English hospital, it was found that RN mean staffing levels (MSLs) was 4.75 HPPD, with high variation within and between wards. For National Early Warning Score” (NEWS) values >7, RN Hours per Patient Day (HPPD) levels (and not NA-HPPD levels) was significantly associated with ‘failure to respond’ to patients with markedly disordered physiology. Likewise, the mean response rate for NEWS values >7 (expected response within 4h) was lower than that >6 (84%; expected response within 16h).Thus, this suggests that mostly critically-ill patients depend on RN-staff and not HCA-staff. However, RN-staff have less time with patients-per-day, hence, they can’t respond to patients quickly and give optimum-care, which resulted in 4.1% mortality-rate; as patient-to-RN ratios are high. Also, no linear interactions between NA- and RN-staff, thus, disputing the claim that NA-staff act as a substitute for RN, or complement the workload of RN-staff to enable them to attend to more patients. Notably, authors could not establish a relationship between ‘failure to respond’ and the RN- or NA-SLs for patients with NEWS values >6.
Qualitative research was used to collect reports for both studies and the findings match their aims as the studies shed more light about patient dissatisfaction and how they patients received a lower quality-of-care due to low RN-SLs being allocated to higher patient numbers, hence, safe staffing levels for optimum-care was not established (NICE, 2014).
However, Unison 2017 case study is similar to Bridges et al, 2019, in terms of patient-to-staff ratios, it describes that patient-to-staff ratios affect patient safety and quality of care. Although Unison (2017), used survey method to collect data. The finding of the study matches the aim of the study as they found out that during the shifts where a nurse cared for > eight patients, adverse-outcomes were increased due to high patient- to staff-ratios.
A similarity of these studies is that participants chosen are elderly participants with comorbidities, depicting that care was important and showing the severity that low RN-SLs cost patient-outcomes, likewise, majority of the participants were female. Likewise, large samples were included in Unison, 2017 and Smith et al., 2020, but small sample size was used in Bridges et al., 2019. Though, all three studies had a degree of variable data i.e. Unison, 2017 and Smith et al., 2020 were done in different wards in one hospital and Bridges et al., 2019 was done in six wards in two hospitals. However, due to the lack of large sample size and restriction to one hospital in respective studies, it is difficult to generalise the data to the greater English-population.
THEME 2: Missed Care
Two main studies covered this theme (Aiken et al., 2017; Griffith et al., 2018).
Aiken et al., 2017 carried out an observational study to research how nursing-SLs are associated with patients’ perceptions and ratings of hospital-care using nurse and patient data from 2010 NHS survey. From the survey, 60% of patients rates that their care was always excellent and there was always adequate RNs and doctors to care from them. However, 17% stated that there was an always inadequate nurse available for care, and 3% stated that there were neither adequate doctors nor RNs available for care. Notwithstanding, these values show that patients view nurses’ quality-of-care and professionalism as of quite similar significance as doctors.
In a retrospective, longitudinal observational study, Griffith et al. (2018), reports were given about how adverse-outcomes are associated with low nursing-SLs, with respect to RNs and HCAs, in relation to skill-mix. It was found that higher levels of missed observations were associated with lower RN-SLs and vice versa. Hence, indicating a dose-response relationship between the two factors.
In Aiken et al., 2017,variations were found in patient-to-nurse ratios/workload across NHS general acute-hospitals suggesting how severe missed nursing-care is and affects patients, and shows the broad differences in variation between hospitals on RN-SLs are. Likewise, Griffith et al., 2018 lays emphasis on the hours worked. Lower rates of missed observations was significantly associated with higher RN-HPPD and HCA-HPPD. Higher admissions-per-RN correlated strongly with significantly higher missed observations rates. However, the advantages of extra HCA hours i.e. 5% decrease in missed observations only existed when RN-HPPD was low.
These findings are supported by past research that higher patient-to-RN workload is associated with adverse patient-outcomes e.g. higher in-hospital mortality – (Ball et al., 2018; Griffith et al., 2016; Rafferty et al., 2007).
The patient-to-staff ratios in these studies linked to more missed care are high and above the recommended threshold by NICE and the NHS (NICE, 2014; NHS Improvement, 2018). Thus, recommended interventions to improve quality-of-care and patient satisfaction is to set compulsory maximum limits on patient-to-staff ratios like that adopted from initiatives in Wales in order to provide safe and efficient nursing-care for patient-outcomes.
Another strategy to improve nursing-care and nursing-outcomes is improving the work-environment. As reported in Aiken et al., 2017, in hospitals where work-environment is quite unfavourable for nurses, missed care occurred more and made patients’ views on care quite unfavourable. Empirical evidence has suggested some less-expensive and economic interventions involving RNs working in supportive hospital work-environments, with adequate equipment and medications, which boosts efficient and safe nursing-care to patients and produce higher patient-outcomes at relatively cheap cost. (Kutney-Lee et al., 2015; Silber et al., 2016; Tucker and Spear, 2006)
Both studies achieved their aims, Aiken et al., 2017 showed how patient satisfaction is influenced by nurse-staffing levels, missed nursing-care and hospital work-environment, and suggested strategies to improve nursing-care, patient-outcomes and nursing work-environments. Griffith et al., 2018 gave reports on independent longitudinal relation of RN-SLs and Na-SLs to patient-outcomes. Aiken et al., 2017 used validated measurements for nurse-staffing, patient satisfaction, missed nursing care and hospital a work environment from many NHS hospitals.
Advantage of these studies is that they both included English NHS hospitals; hence data can be comparable as hospitals used are under the same healthcare policy. They both included large number of participants: 66,348 hospital patients (Aiken et al., 2017) and 138,133 patients (Griffith et al., 2018). The number of nurses was stated in Aiken et al., 2017, however, the hours of shifts was included in Griffith et al., 2019.
However, Aiken et al. (2017) used survey data from 2010. A critique is that such data is old and healthcare policies have changed within 8 years. However, authors argued that till-date this is the only comprehensive data that discusses the association between nurse-SLs/workload and patient satisfaction, using data from many English hospitals. This notion can be supported by findings in Griffith et al. (2018) and reports from healthcare policy-makers, which suggests that finding the balance between nurse-SLs, quality-of-care and patient-outcomes is still an ongoing target, although soon to be rectified in the near future (House of Commons Health Committee, 2018).
Both studies have shown that missed care is a good indicator for inadequate staffing. Particularly, missing vital signs observations is an important mechanism for this association, as its been shown that such mechanism is associated with vital patient-outcomes and developing adequate nurse-SLs (Griffith et al., 2018).
THEME 3: Mortality
Four main studies covered this theme (Dall’Ora et al., 2019; Griffith et al., 2018; Griffith et al., 2019; West et al., 2014).
In a retrospective-longitudinal-study, Griffith et al. (2019), the hospital-mortality was 4.1%. The hazard-of-death (HoD) correlated more with RN-staff than NA-staff. Each day a patient encountered a RN below ward-mean, the HoD increased by 3% and there was a 3% decrease in HoD (relative to ward-mean) for each hour an RN was available over the first 5 days of a patient-admission.
A linear relationship between RN levels and mortality was reported; 125% increase of ward-mean for admission-per-RN, correlated with a 5% HoD increase on such days. However, across wards, mean-staffing-level (MSL) per-day was 4.75 RN-hours-per-patient and 2.99 NA-hours-per-patient, with mean-skill-mix of 61% RN-staff; hence, higher percentage of RN-staff explains the relatively low mortality-rate.
Likewise, in the similar study that included HCAs, Griffith et al., 2018, HoD increased by 3% each day a patient was on a ward where RN-staffing-levels (RN-SLs) were below the mean and there was a 4%HoD increase each day a patient was exposed to HCA-staffing-levels (HCA-SLs) below the mean. Thus, this suggests that low-staffing-levels (low-SLs) of nurses is associated with increased adverse-outcomes. Similarly, HoD increased by 9% for each day RN-HPPD decreased below the estimated RN-establishment but no statistically significant association with HCA-staffing. Thus, lower RN-SLs per-admission are linked with adverse-outcomes especially mortality and the patients who experience higher-staffing have reduced length-of-stay on hospital-ward, whereas non-linear relationship was associated with HCA-SLs, though a slight negative-effect was found on length-of-stay.
West et al., 2014 also reported that higher number of consultants and nurses per-bed increased the survival-rates of those critically-ill hospital-patients. Also, no dissimilarities in survival-rates for ICU patients associated with doctors or nurses. It also highlights a key principle easily forgotten, is the importance of teamwork. For example, Kim et al., 2010 suggests that decreased mortality-rates in ICU-units was associated with daily rounds of a multi-disciplinary team (physicians, nurses, respiratory therapists, clinical pharmacists, social workers etc).
Accordingly, Griffith et al., 2019 suggests that non-linear relationship with NA staff and admitted patients’ risk of death was recorded: low NA staffing was associated with increased risk of mortality and high NA staffing with increased mortality. Thus, this opposes the view that NA staff in place of low RN levels helps improve patient outcome (Aiken et al., 2013; Duffield et al., 2011; Estabrooks et al., 2005). Similarly, West et al., 2014 reported that there was no evidence that the support-staff working in the unit increased patient survival/outcomes, although they might have made it easier for RNs to provide sufficient patient-care.
Thus, this suggests that inadequacy in improving patient-outcomes and mortality is because of division-of-labour i.e. low RN-to-patient ratio means RN-staff reducing scheduled and spontaneous patient observation and assessment (Twigg et al., 2016).
Similarly, West et al., 2014, stated that high-workload for nurses i.e. low nurses-to-patient ratios was associated with increased in-hospital mortality. The significant association between nurse-SLs and patient-mortality-risks suggests that an increase in nurses availability significantly affects those at greatest risk-of-death.
In terms of temporary staffing, Griffith et al., 2019 found that 12% HoD increase on days patients were exposed to ≥1.5 HPPD of temporary-RN-staffing and a linear-relationship; increased length-of-exposure for patients to low RN-SLs significantly increased HoD. These findings were supported by Dall’Ora et al., (2019), that also stated that at any level, temporary-NA-staffing was linked to high-risk of patient dying, high temporary-NA-SL effects was lower than that of high temporary-RN-SLs. Thus, this emphasises the importance of having high levels of permanent-RN-staff who are more adaptable to the work environment, unit practices, patients and workload, hence, capable of enforcing patient safety and optimum care.
These observational studies meet their aims as they show the influence of types of nurse-staffing on nursing-care and resultantly mortality, and considered patient encounters/experiences with staffing-levels whilst considering risk-of-death.
The measurements used by Griffith et al., (2018, 2019) to generate MSLs, was the evidence-based common staffing-methodology, Safer Nursing Care Tool (The Shelford Group, 2014), endorsed from NICE (NICE, 2014) which indicated a possible optimum NA-SL to compensate for low RN-staffing because the HoD was low when staffing was close to this level. Although, with slight deviations, for man staffing-levels there was a significant association between planned and actual staffing levels. However, the needed daily variation are unlikely to be reflected by such planned staffing levels. Therefore, to define sufficient staffing, it is unclear whether staffing clarificationsfocused on everydayevents using this tool are efficient or instead routinely-collected data e.g. NEWS.
However, these studies were retrospective studies and relied on past collected-data, hence, it is questionable if such data relates to current hospital practice. Yet, reports on healthcare policies suggests that not much change has been made (House of Commons Health Committee, 2018).
Likewise, all the studies were done in a single hospital respectively, although many patients were accessed and different wards were put into consideration, this shows that the finding give the ‘in-hospital’ effect, however, as one trust/hospital was used, generalizability to other hospitals, patients and nursing-staff in other UK locations is limited.
DISCUSSION
The first theme that is evident in the literature review conducted is staff-to-patient ratio in most acute care hospitals. The number of registered nurses in such institutions is worrying, which breeds a bigger problem of low service provision. Having few registered nurses has made many people to experience missed care (Dall’Ora et al., 2019; Griffith et al., 2018; Griffith et al., 2019; West et al., 2014). Missed care within healthcare facilities leads to death of patients who could otherwise be saved. There is an urgent need to address the shortage that is being experienced in the United Kingdom in a bid to reduce damage that can be felt within the society. Most studies have noted that healthcare problems being experienced can be handled by reducing the gap between nurses and patients that are admitted to acute care hospitals (Buchan et al., 2019; House of Commons Health Committee, 2018). Insufficient nurse registration denies the public basic services due to lack of adequate staff to extend their services throughout the country. Low staffing in acute care hospitals leave patients neglected and unattended to as indicated by the literature review conducted.
The second theme that is evident is missed care for patients who are in critical conditions in acute care hospitals. Missed care is as a result of neglect to patients who are suffering from serious conditions. A patient under cute care should not miss on basic care that can boost the recovery process within such institutions (Dall’Ora et al., 2019; Griffith et al., 2018; Griffith et al., 2019; West et al., 2014). The missed care has led to fatal circumstances and there is need to address the issue with skepticism as a way of devising a strategic approach. Failure for healthcare institutions to heed to increased staff requirements might subject the country into more deaths as studies suggest (Buchan et al., 2019; House of Commons Health Committee, 2018). It is important to note that patients who are subjected to holistic acre are better placed to recover as compared to neglected ones. Missed care is an evident theme in the literature review conducted on the effect of insufficient nurse staffing to provision of care within acute hospitals in the UK.
The third theme evident is mortality as a result of neglected care or lack of proper medication. The number of registered nurses is low prompting the system to utilize the available personnel in a bid to provide quality service (Buchan et al., 2019; House of Commons Health Committee, 2018). Due to the high number of patients, the care provides are not able to handle all patients as required. In the event, some patients miss the necessary care that can help them recover and eventually die. Low staffing of nurses contributes to a significant mortality rate within the United Kingdom. Studies suggest that in hospitals where there is a low patient to staff ratio, care provision is improved as compared to institutions that have less nurses (Stimpfel et al., 2015). When a patient misses care due to inadequate staff, they are likely to die due to neglect and lack of proper care. As such, mortality experienced in acute care hospitals within the United Kingdom might be as a result of insufficient nurse staffing.
A discussion on the three themes is important as it enlighten the society where the problem lies for acute care hospitals. For instance, it is through low nurse registrations that many patients experience missed care leading to death. The three are discussed as they are interrelated and that one problem leads to the other (Buchan et al., 2019; House of Commons Health Committee, 2018). Insufficient nurse registration is posing a challenge and has resulted to a larger percentage of the missed care in acute hospitals. The missed care in turn can lead to severity of a condition or death as it is in most cases (Stimpfel et al., 2015). A discussion of the three helps find the precise problem that has plagued provision of quality healthcare services to people.
To address the issue of low nurse registration within the United Kingdom, all stakeholders must act promptly and fix the mess. For instance, the government can increase the number of students who are enrolled yearly to undertake nursing courses in learning institutions (Buchan et al., 2019; House of Commons Health Committee, 2018). Equally, it is the duty of healthcare institutions to make the environment conducive in a bid to attract professional nurses. The government should be at the forefront of ensuring that the right strategies are deployed to guarantee improved care within the UK.
* Training programs for nurses should be implemented across the world to boost service delivery. More resources should be put into this field to ensure that patients are handled in the right manner. The fewer the number of registered nurses, the less the amount of healthcare provision that patients can receive (Buchan et al., 2019; House of Commons Health Committee, 2018). A desirable ration of nurse to patients guarantees paper care, which is required for faster recovery. Training and developmental programs for all nurses within the United Kingdom can help establish various facts that can promote healthcare provision. The NHS should spearhead changes in the healthcare sector in a bid to streamline operations for better service delivery. As a long-term plan, the NHS intends to apply the new magnet model to boost attractiveness of working places for professional nurses. To make such places attractive requires satisfying salaries for practitioners (Buchan et al., 2019; House of Commons Health Committee, 2018). The NHS should put more action in reducing inequalities that are notable in the United Kingdom. Equally, investing in research can prove an important matter as it can help determine areas where the system has failed in providing the required care. Failure to revisit policies in place can subvert further attempts to achieve improved patient care in acute hospitals within the United Kingdom. However, implementation of such policies requires resources and commitment for it to bear fruit. It is always better to ensure prevention of a particular issue than handling its cure. The NHS has an obligation to coordinate the other stakeholders in the sector to spearhead the necessary changes in healthcare.
In consideration to theories of communication in nursing, it is critical to apply the right strategies in the process of relaying information. The theory of communication in nursing is based on the fact that nurse-client relationship is critical for one to recover. In situations where communication is poor between a patient and the nurse, one fails to open up on issues that could be a stumbling block to recovery (England HE, 2017; Willis, 2015). Proper care and communication makes patients trust nurses, which aids them to heal faster. The quality of life one is accorded while sick determines how fast they can recover and adapt to the state. As such, nurses play a critical role in delivering holistic care in various facilities and it is in order that they are involved in policy formulation process.
The level of change expected should cover the whole United Kingdom as a society in a bid to reduce inequalities in the healthcare sector (England HE, 2017; Willis, 2015). As such, it requires proper planning to avoid wastage of resources, which could otherwise be used to hire more nurses. Policies that affect the sector are formulated at a national or international level after a thorough consultative process. When policies affect a whole society, one facility cannot come up with rules of operations without involving the rest of the stakeholders. The importance of consulting is to have a way of accessing funds for implementation of such policies. The NHS should be at the forefront of nationwide changes for a better future in the healthcare sector. Initiating changes within the healthcare sector requires resources and input from all involved parties for goals to be achieved. A facility should always consider some factor before deciding on adopting the changes within its operations.Hence, this is a cost-effective intervention for NHS policy-makers to adopt to improve working-environments, reduce patient-to-staff ratios, improve nursing-care quality and thus, diminish adverse patient-outcomes.
RECOMMENDATIONS
A recommendation relating to data-collection tools would be that future studies should use more evidence-based tools e.g. the Safer Nursing Care Tool used in Griffith et al., (2018, 2019), which was associated with better patient-outcomes and decreased length-of-stay.
As suggested in the discussion, there should be more expenses spent in recruiting more RN-staffing as included researches have stressed that this boosts patient-outcomes and nursing care-quality compared to HCA/NA-SLs. Likewise, RNs are cost-effective in the long-run as skill-mix increases, care is improved, and less length-of-stay for patients decreases.
The effects and effectiveness of agency- and hospital-bank staff should also be considered independently because bank staff might be more-skilled and less adverse-outcomes might be associated with them. Hence, knowing this would make training-posts more effective to generate more-skilled staff who can perform RN tasks effectively to reduce workload.
Training for temporary- and NA-staff should not just include ward training; they should also include lecture training, and written and oral examinations as if they are undergoing nursing bachelor’s degree programme. This is to ascertain that the nurses have researched on their field and have been trained academically to give them a broad knowledge about their professional responsibilities. Therefore, nursing becomes their appreciatedprofession, instead of a part-time job to pay their monthly bills.
Implementing the suggested changes within the healthcare sectors requires a thorough assessment to ascertain validity (England HE, 2017; Willis, 2015). It is important that political, social, economic, technological, legal and environmental factors are taken into consideration. Politically, the United Kingdom government is committed to ensure that healthcare provision is improved in the country. Economically, the resources are available to implement various training programs that can help change the face of healthcare provision. The social culture in the United Kingdom can accommodate the changes that are proposed in a bid to promote a desirable population health (England HE, 2017; Willis, 2015). Equally, operations within the sector should be within the set legal limits to avoid any litigation matters. The environment should be attractive and welcoming to professional and experienced nurses for improved service delivery.
It is always important to assess a research to establish its validity and reliability of the facts in the study. A SWOT analysis is an essential tool that can help gain a deeper insight into the issue of insufficient nurses within the United Kingdom. As a strength, the study established crucial aspects that impact the recruitment and training of nurses within the country (Stimpfel et al., 2015). Additionally, new employees take time to adapt and some might fail to adjust to the new working environment. Such aspects form the major weaknesses of establishing changes within the healthcare sector. As an opportunity, the need to have professionals who can deliver quality care in the country makes it necessary for the investment and changes (Aiken et al., 2008). Nurses should advocate for professionalism and inclusion during the decision making processes in the healthcare sector.
CONCLUSION
Included research has shown that the patient’s views on hospital-care has helped to increase importance of the severity of missed nursing-care, which is associated with poor work-environments and low RN-SFs. Thus, improving patient satisfaction, high patient-to-staff ratio, the quality and quantity of patient-nurse interactions, skill-mix, nursing-care and adverse outcome e.g. in-hospital mortality are by-products of increasing NHS hospital RN-SLs. However, heavily relying on temporary- and assistant-staff is associated with higher risk of in-hospital mortality. Though findings show that improving RN-SLs is a huge benefit for in-hospital-care and patient-outcome, in the UK, RN-shortfalls is still a major issue. Long-lasting disparitybetween RN supply and demand, public sector pay limit effects, wider labour market and demographic alternations are responsible for aggravating this issue . However, one NHS trust cannot provide solutions to such continuous problems. Although, the work environments and non-monetary benefits of trusts makes it an attractive employer to nurses, the competition of limited nurses’ supply on compensationterms by employers is prevented by the national pay context.
This has sparked policy-makers’ interests in the ‘Magnet Hospitals’ model, which is a concept which achieved professional nurse attraction, recruitment and retention through its improved work environments. Past research have also suggested that higher nursing-SLs also potentially decreases nursing turnover and sickness absence associated with fatigue and burnout alongside discovered associations with increased RN-SLs i.e. increased job satisfaction, decreased staff workload, fatigue and burnout and increased staff retention. Thus, further prospective studies in UK on this topic using evidence-based data-collection tools are needed to assist policy-makers in knowing specific locations and in-hospital care and administration that need more attention, to boost better working environments for nurses alongside increasing RN-SLs and thus, improving patient-outcomes.
References
Aiken L.H., Clarke S.P., and Sloane D.M. (2002). Hospital staffing, organization, and quality of care: cross-national findings. Nurs Outlook, 50, 187–94
Aiken L.H., Clarke S.P., Cheung R.B., et al. (2003). Educational levels of hospital nurses and surgical patient mortality. JAMA, 290, 1617–23.
Aiken L.H., Xue Y., Clarke S.P., Sloane D.M. (2007). Supplemental nurse staffing in hospitals and quality of care. The Journal of Nursing Administration, 37, 335–42. Doi: doi: 10.1097/01.NNA.0000285119.53066.ae
Aiken, L., Buchan, J., Ball, J. and Rafferty, A. (2008). Transformative impact of Magnet designation: England case study. Journal of Clinical Nursing, 17(24), pp.3330-3337.
Aiken L, Rafferty AM, Sermeus W. (2014). Caring nurses hit by a quality storm. Nursing Standard, 28, 22–5.
Aiken L.H., Sermeus W., Van den Heede K., Sloane D.M., Busse R., McKee M., et al. (2012). Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. British Medical Journal, 344:e1717. Doi:10.1136/bmj.e1717
Aiken L.H., Shang J., Xue Y., Sloane D.M. (2013). Hospital use of agency-employed supplemental nurses and patient mortality and failure to rescue. Health Services Research, 48, 931–48. Doi:10.1111/1475-6773.1201
Aiken, L., Sloane, D., Bruyneel, L., Van den Heede, K., Griffiths, P., Busse, R et al. (2014). Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. The Lancet, 383(9931), pp.1824-1830.
Aiken, L., Sloane, D., Ball, J., Bruyneel, L., Rafferty, A. and Griffiths, P. (2017). Patient satisfaction with hospital care and nurses in England: an observational study. BMJ Open, 8(1), p.e019189.
Aiken, L., Sloane, D., Griffiths, P., Rafferty, A., Bruyneel, L., McHugh, M., Maier, C., Moreno-Casbas, T., Ball, J., Ausserhofer, D. and Sermeus, W. (2016). Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Quality & Safety, 26(7), pp.559-568.
Allan HT, Magnusson C, Evans K, Ball E, Westwood S, Curtis K, et al. (2016) Delegation and supervision of healthcare assistants’ work in the daily management of uncertainty and the unexpected in clinical practice: invisible learning among newly qualified nurses. Nursing Inquiry, 23, 377–85. Doi: 10.1111/nin.12155
Alvarez, M. R., Kerr, B. J., Jr., Burtner, J., Ledlow, G., & Fulton, L. V. (2011). Use of outsourced nurses in long-term acute care hospitals: Outcomes and leadership preferences. Journal of Nursing Administration, 41(2), 90–96. Https://doi.org/10.1097/ NNA.0b013e31820594a8
Ausserhofer D, Schubert M, Desmedt M, Blegen MA, De Geest S, Schwendimann R (2013). The association of patient safety climate and nurse-related organizational factors with selected patient outcomes: a cross-sectional survey. International Journal of Nursing Studies, 50,240–52. Doi: 10.1016/j.ijnurstu.2012.04.007
Bae, S. H., Brewer, C. S., Kelly, M., & Spencer, A. (2015). Use of temporary nursing staff and nosocomial infections in intensive care units. Journal of Clinical Nursing, 24(7–8), 980–990. https:// doi.org/10.1111/jocn.12718
Bae, S. H., Kelly, M., Brewer, C. S., & Spencer, A. (2014). Analysis of nurse staffing and patient outcomes using comprehensive nurse staffing characteristics in acute care nursing units. Journal of Nursing Care Quality, 29(4), 318–326. https://doi. org/10.1097/NCQ.0000000000000057
Ball, J., Bruyneel, L., Aiken, L., Sermeus, W., Sloane, D., Rafferty, A., Lindqvist, R., Tishelman, C. and Griffiths, P. (2018). Post-operative mortality, missed care and nurse staffing in nine countries: A cross-sectional study. International Journal of Nursing Studies, 78, pp.10-15.
Bloom JR, Alexander JA, Nuchols BA. (1997). Nurse staffing patterns and hospital efficiency in the United States. Social Science and Medicine, 44, 147–55. Doi:10.1016/S0277-9536(96)00063-9
Bridges, J., Griffiths, P., Oliver, E. and Pickering, R. (2019). Hospital nurse staffing and staff–patient interactions: an observational study. BMJ Quality & Safety, 28(9), pp.706-713.
Buchan J, Seccombe I, Gershlick B, Charlesworth A. (2017) In Short Supply: Pay Policy and Nurse Numbers. London: Health Foundation.
Buchan J., Charlesworth A., Gershlick B., and Seccombe (2019). A critical moment: NHS staffing trends, retention and attrition. London: The Health Foundation
Cardona-Morrell M, Prgomet M, Turner RM, Nicholson M, Hillman K. (2016). Effectiveness of continuous or intermittent vital signs monitoring in preventing adverse events on general wards: a systematic review and meta-analysis. International Journal of Clinical Practice, 70, 806–824. Doi:10.1111/ijcp.12846
Collins A. (2018). NHS will still be short of nurses in five years, Dalton warns. Nursing Standard, 20 December 2018. Accessed: 20/01/2020 Available from: https://www.nursingtimes.net/news/workforce/nhs-will-still-be-short-of-nurses-in-five-years-warns-regulator-chief-20-12-2018/
Dall’Ora, C., Mauotti, A., and Griffiths, P. (2019). Temporary Staffing and Patient Death in Acute Care Hospitals: A Retrospective Longitudinal Study. Journal of Nursing Scholarship. https://doi.org/10.1111/jnu.12537
Department of Health and Human Services. (2016). New nursing degree apprenticeship United Kingdom: GOV.UK. [Accessed: 23/01/2020] Available from: https://www.gov.uk/ government/news/new-nursing-degree-apprenticeship
Duffield, C., Diers, D., O’Brien-Pallas, L., Aisbett, C., Roche, M., King, M. and Aisbett, K. (2011). Nursing staffing, nursing workload, the work environment and patient outcomes. Applied Nursing Research, 24(4), pp.244-255.
Dunn, D. (2014).Where oh where are the OR nurses? ORNurse Manager, 8(3), 8–
England H.E. (2017). Facing the facts, shaping the future: a draft health and care workforce strategy for England to 2027. London: Health Education England.
Estabrooks, C., Midodzi, W., Cummings, G., Ricker, K. and Giovannetti, P. (2005). The Impact of Hospital Nursing Characteristics on 30-Day Mortality. Nursing Research, 54(2), pp.74???84.
Flinkman, M. ,Isopahkala-Bouret, U. , Salantera, S. (2013).Young registered nurses’ intention to leave the profession and professional turnover in early career: a qualitative case study. ISNR Nursing, 916061
Ganeshkumar P, Gopalakrishnan S. (2013). Systematic reviews and meta-analysis: Understanding the best evidence in primary healthcare. Journal of Family Medicine and Primary Care, 2(1),9.
Griffiths, P., Ball, J., Drennan, J., Dall’Ora, C., Jones, J., Maruotti, A., et al. (2016). Nurse staffing and patient outcomes: Strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for the National Institute for Health and Care Excellence Safe Staffing guideline development. International Journal of Nursing Studies, 63, pp.213-225.
Griffiths, P., Ball, J., Murrells, T., Jones, S. and Rafferty, A. (2016). Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: a cross-sectional study. BMJ Open, 6(2), p.e008751.
Griffiths, P., Maruotti, A., Recio Saucedo, A., Redfern, O., Ball, J., Briggs, J., Dall’Ora, C., Schmidt, P. and Smith, G. (2019). Nurse staffing, nursing assistants and hospital mortality: retrospective longitudinal cohort study. BMJ Quality & Safety, 28(8), pp.609-617.
Francis R. (2013). Report of the mid staffordshire NHS foundation trust public inquiry. [Accessed: 22/01/2020]. Available from: http://webarchive.nationalarchives.gov.uk/2015 0407084003/http://www.midstaffspublicinquiry.com/report
Handbook-5-1.cochrane.org. (2020). 4 Assessment of study quality and risk of bias. [online] Available at: https://handbook-5-1.cochrane.org/chapter_21/21_4_assessment_of_study_quality_and_risk_of_bias.hm [Accessed 29 Jan. 2020].
Griffiths P, Ball J, Bloor K, et al. (2018). Nurse staffing levels, missed vital signs and mortality in hospitals: retrospective longitudinal observational study.Southampton NIHR Journals Library. Health Services and Delivery Research, No. 6.38. Southampton (UK): NIHR Journals Library; 2018 Nov.
Griffiths P., Saucedo A., Dall’Ora C., Briggs J., Maruotti A., Meredith P., et al. (2018). The association between nurse staffing and omissions in nursing care: a systematic review. Journal of Advanced Nursing, 74, 1474–87. Doi:10.1111/jan.13564
House of Commons Health Committee. (2018). The Nursing Workforce: Second Report of Session 2017–19. TSO (The Stationery Office).
Hurst K., Smith A. (2011). Temporary nursing staff – cost and quality issues. Journal of Advanced Nursing, 67(2), 287–96. Doi:10.1111/j.1365-2648.2010.05471.x
Keogh B. (2013). Review into the quality of care and treatment provided by 14 hospital trusts in England: overview report. [Accessed: 22/01/2020]. Available from: http://www.nhs.uk/NHSEngland/bruce-keogh-review/Documents/ outcomes/keogh-review-final-report.pdf
Kane, R., Shamliyan, T., Mueller, C., Duval, S. and Wilt, T. (2007). The Association of Registered Nurse Staffing Levels and Patient Outcomes. Medical Care, 45(12), pp.1195-1204.
Kim, M.M., Bernato, A.E., Angus, D.C., Fleisher, L.F., Kahn, J.M., (2010.) The effect of multidisciplinary teams on Intensive Care Unit mortality. Archives of Internal Medicine, 170 (4) 369–376.
Kutney-Lee, A., Stimpfel, A., Sloane, D., Cimiotti, J., Quinn, L. and Aiken, L. (2015). Changes in Patient and Nurse Outcomes Associated With Magnet Hospital Recognition. Medical Care, 53(6), pp.550-557.
Mcclure ML, Poulin MA, Sovie MD, Wandelt MA. (1983). Magnet Hospitals: Attraction and Retention of Professional Nurses. Task Force on Nursing Practice in Hospitals. American Academy of Nursing. Kansas City, MO: American Nurses Association Publications.
Monahan, J. (2015). A Student Nurse Experience of an Intervention that Addresses the Perioperative Nursing Shortage. Journal of Perioperative Practice, 25(11), pp.230-234.
National Advisory Board on the Safety of Patients in England. (2013). A promise to learn–a commitment to act: improving the safety of patients in England. London: Department of Health. [Accessed: 23/01/2020]. Available from: www. health.org.uk/government/publications/berwick-review
National Institute for Health and Care Excellence (NICE). Safer Nursing Care Tool (SNCT): Statement of Endorsement. London: NICE; 2014.
NHS Digital. (2018) NHS Workforce Statistics – July 2018. NHS Digital, 2018 [Accessed: 22/01/2020]. Available from: https://digital.nhs.uk/data-andinformation/publications/statistical/nhs-workforce-statistics/nhs-workforce-statistics—october-2018-provisionalstatistics
NHS Improvement. (2018). Staff Retention Support Programme: One Year On. NHS Improvement, 2018 [Accessed: 22/01/2020]. Available from: https:// improvement.nhs.uk/resources/staff-retention-support-programme-one-year
NICE, 2014. Overview | Safe staffing for nursing in adult inpatient wards in acute hospitals | Guidance | NICE. [online] Available at: https://www.nice.org.uk/Guidance/SG1 [Accessed 30 Jan. 2020].
Petersen JA, Antonsen K, Rasmussen LS. (2016). Frequency of early warning score assessment and clinical deterioration in hospitalized patients: a randomized trial. Resuscitation, 101, 91–6. Doi:10.1016/j.resuscitation.2016.02.003
Rafferty, A., Clarke, S., Coles, J., Ball, J., James, P., McKee, M. and Aiken, L. (2007). Outcomes of variation in hospital nurse staffing in English hospitals: Cross-sectional analysis of survey data and discharge records. International Journal of Nursing Studies, 44(2), pp.175-182.
Recio-Saucedo A, Dall’Ora C, Maruotti A, Ball J, Briggs J, Meredith P, et al. (2018). What impact does nursing care left undone have on patient outcomes? Review of the literature. Journal of Clinical Nursing, 27, 2248–59. Doi:10.1111/jocn.14058
Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, De Geest S (2008). Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. International Journal of Quality Health Care, 20, 227–37. Doi:10.1093/intqhc/mzn017
Silber, J., Rosenbaum, P., McHugh, M., Ludwig, J., Smith, H., Niknam, B., Even-Shoshan, O., Fleisher, L., Kelz, R. and Aiken, L. (2016). Comparison of the Value of Nursing Work Environments in Hospitals Across Different Levels of Patient Risk. JAMA Surgery, 151(6), p.527.
Smith R. (2012). Nurses lack compassion NHS admits. The Telegraph. [Accessed: 22/01/2020]. Available from: https://www.telegraph.co.uk/news/health/news/9020360/Nurses-lack-compassion-NHS-admits.html
Smith, G., Redfern, O., Maruotti, A., Recio-Saucedo, A. and Griffiths, P. (2020). The association between nurse staffing levels and a failure to respond to patients with deranged physiology: A retrospective observational study in the UK. Resuscitation.
Sochalski J. (2004). Is more better?: the relationship between nurse staffing and the quality of nursing care in hospitals. Medical Care, 42, II-67-II-73.
Stimpfel, A., Sloane, D., McHugh, M. and Aiken, L. (2015). Hospitals Known for Nursing Excellence Associated with Better Hospital Experience for Patients. Health Services Research, 51(3), pp.1120-1134.
The Shelford Group. (2014). Safer nursing care tool implementation resource pack. The Shelford Group.
Tucker AL, Spear SJ. (2006). Operational failures and interruptions in hospital nursing. Health Services Research, 41, 643–62.
Twigg, D., Myers, H., Duffield, C., Pugh, J., Gelder, L. and Roche, M. (2016). The impact of adding assistants in nursing to acute care hospital ward nurse staffing on adverse patient outcomes: An analysis of administrative health data. International Journal of Nursing Studies, 63, pp.189-200.
UNISON, 2017. Ratios not rationing, UNISON safe staffing report 2017. [Accessed: 07/01/2020]. Available from: https://www.unison.org.uk/content/uploads/2017/04/Rationotrationing.pdf
West, E., Barron, D., Harrison, D., Rafferty, A., Rowan, K. and Sanderson, C. (2014). Nurse staffing, medical staffing and mortality in Intensive Care: An observational study. International Journal of Nursing Studies, 51(5), pp.781-794.
Willis G. (2015). Shape of caring: a review of the future education and training of registered nurses and care assistants. London: Health Education England.
Wu, S. H., & Lee, J. L. (2006). A comparison study of nursing care quality in different working status nursing staffs: An example of one local hospital. Journal of Nursing Research, 14(3), 181–189.
Xue, Y., Aiken, L. H., Freund, D. A., & Noyes, K. (2012). Quality outcomes of hospital supplemental nurse staffing. Journal of Nursing Administration, 42(12), 580–585. https://doi.org/10.1097/NNA.0b013e318274b5b
Yakusheva O., Lindrooth R., Weiss M. (2014). Economic evaluation of the 80% baccalaureate nurse workforce recommendation: a patient-level analysis. Medical Care, 52, 864–9