Research Paper on a Validation of Diagnostic Criteria for Severe Sepsis and Sepsis Management
Number of words: 4041
Table of Contents
| Chapter 1: Introduction | 1 |
| Research objectives | 2 |
| Hypotheses | 2 |
| Significance of the study | 2 |
| Literature Review | 3 |
| Chapter 2: Methods | 5 |
| Research design | 5 |
| Locale of the study | 5 |
| Participants | 5 |
| Instrumentation | 5 |
| Data gathering procedure | 11 |
| Data analysis | 11 |
| Ethical Consideration | 12 |
| References | 13 |
Chapter 1: Introduction
Over the years, the clinical understanding of sepsis has evolved as physicians seek to identify and explain the pathophysiology of this severe condition. The term sepsis derives its meaning from the Greek word “sepo,” which means to decay or decompose (Gary et al. 2016). Therefore, sepsis is a life-threatening immunological condition that occurs when microorganisms enter the human body, causing a severe internal response that poses the danger of malfunction to major body organs, sepsis shock, and death. In critically ill patients, sepsis is a major trigger for death, making the condition a primary cause of mortalities associated with kidney failure, heart attack, and paralysis. According to Gyawali et al. (2019), the incidence rate of mortalities associated with severe sepsis and septic shock is about 300 in every 100,000 people in the U.S. alone. Although the global impact of sepsis is difficult to establish, it is estimated that in every year, approximately 30 million people worldwide develop a septic infection, leading to about 6 million deaths (Reinhart 2017).
The diagnosis of sepsis is often difficult to determine, given that its symptoms are closely linked to those of other medical conditions at its early stages. The main signs and symptoms include low blood pressure, severe fever, abnormal heart rate, and obstructive breathing. Patients with organ dysfunction resulting from secondary factors other than an infection face the risk of misdiagnosis, especially if their condition comes as an emergency (Fan et al. 2016). Unfortunately, there lacks a clear indicator that can singly identify the root source of organ failure or shock to a septic attack, according to Zhang (2015). Such clinical misdiagnosis can easily mislead physicians to administer antibiotics to patients under critical care, such as the intensive care unit (ICU), leading to untimely death or permanent organ failure. Worse still, inappropriate subjection of patients to strong doses of antibiotics may lead to the development of drug resistance, which undermines future efforts by doctors to prescribe antibiotic drugs to patients suffering from other diseases.
The implications of mortalities caused by sepsis have made experts in the medical field work hard to uncover the cellular and molecular nature of sepsis-causing infections. Berg & Gerlach (2018), in their review of the current advances in understanding sepsis, point out that the complexity of the pathophysiological pathways of a septic infection is a significant challenge in the timely diagnosis and treatment of sepsis. In most cases, a septic attack occurs as an emergency that requires an immediate medical response, without which patients face the risk of acute kidney failure, heart attack, or even death. However, the Surviving Sepsis Campaign (SSC) has provided international guidelines that physicians should embark on in the management of sepsis. The SSC panel of 2016 comprised of 55 medical experts from 25 international bodies tasked with reviewing the previous guidelines of 2012 (Rhodes et al. 2017). After a series of objective conventions and teleconferences, the committee arrived at a consensus and provided 93 statements on the control and resuscitation of patients with sepsis. In total, strong recommendations, weak recommendations, and best-practice statements were 32, 39, and 18, respectively. The purpose of developing international strategies on sepsis management by SSC was to improve the recovery rate for critically ill patients and to reduce deaths attributed to severe sepsis and septic shock (Weiss et al. 2020).
Several controversies exist between experts on how the diagnosis for sepsis should be carried out. Unfortunately, the lack of agreeable grounds on how to predict the reliability of a biomarker of sepsis infection has remained a significant hindrance to therapeutic approaches towards severe septic attacks (Berg & Gerlach 2018). According to DeVos (2018), diagnostic measures should include a series of intense laboratory tests that can predict the emergence of both mild and acute organ dysfunction. They propose that of equal importance is the ability to control the source of infection and to suppress critical symptoms by using antimicrobial medication. However, Yoo et al. (2015) recommend a slightly different approach. They suggest that since most infections occur when microorganisms in the blood cause an inflammatory response, blood lactate from patients in the intensive care unit is a stronger pointer to establishing the source of septic infection and the amount of antibiotic dosage required for the resuscitation of patients with sepsis. Nevertheless, an overall opinion across most studies is that proper diagnosis of sepsis is necessary for reducing mortalities associated with adverse bodily responses to microbiota in the blood.
As a result, the objective of this study will be to examine the diagnostic measures that physicians in intensive care units apply in classifying severe sepsis and the processes involved in sepsis management. The association between the clinical competency of medical practitioners and mortalities resulting from misdiagnosis and non-adherence to the international guidelines of SSC will also be examined.
Research objectives
Through our research, we aim to contribute towards expounding the knowledge about the management of severe sepsis, hence contributing to the reduction of mortalities associated with sepsis. Our specific objectives will be stated as follows:
- To determine the knowledge and skills of health care practitioners in the management of sepsis
- To identify significant differences on the knowledge and skills of health care practitioners, and
- Based on the findings, determine the areas of improvement in severe sepsis management
Hypotheses
In achieving the objectives of this research, we predict that the following condition will be satisfied to serve as valid diagnostic criteria for severe sepsis and sepsis management.
- Since we postulate that mortality rates are highly associated with clinical incompetency’s, there will be a significant difference between the diagnostic measures used by physicians in managing sepsis and the procedures outlined in the updated guidelines of Surviving Sepsis Campaign.
Significance of the study
The first step towards mitigating critical illnesses that lead to medical emergencies or fatal ends is understanding the nature of the sources of such diseases (Weiss et al. 2020). Through this research, we endeavor to contribute to the pre-existing knowledge of sepsis, and by validating diagnostic measures of severe sepsis, we will add significant value to the understanding of how sepsis attacks occur and how they can be effectively controlled. Therefore, this investigation will shed more light on the physiological nature of sepsis, and will hopefully benefit all who review our research with the aim of understanding sepsis and its management.
In Saudi Arabia, septic shock has been termed by several studies as a significant contributor to neonatal deaths and mortalities among the elderly. One such study was carried out by Gasim (2016) in Buraidah Central Hospital, where a high incidence of deaths related to sepsis was prevalent among patients with respiratory infections. According to Gasim’s study, mortalities due to severe sepsis and septic shock were over 40%, leading to the conclusion that the most affected category of patients was the older people with pre-existing medical conditions, such as pulmonary and respiratory infections. However, Gasim (2016) also observed that there was a significant difference between survivors and those who succumbed to septic shock, whether mechanically ventilated or not. Such an observation indicates that one of the five sections of our hypothetical study, as derived from SSC, may play a role in contributing to sepsis deaths. This analyses by Gasim and other studies point out that there exists a significant knowledge gap among medical officers and the community at large on the appropriate measures for the management of sepsis. Our aim, therefore, is to bridge the gap by exploring the international guidelines outlined by SSC as measures for early sepsis detection and the effective resuscitation of patients with sepsis. By focusing on the incidences of sepsis attacks among patients in a government hospital in Medina, we will identify and highlight the measures that physicians use in diagnosing sepsis, the immediate actions taken to manage septic shock, and how medical incompetency (or competency) contributes to sepsis mortalities (or survival).
Based on the findings of our study, a better and comprehensive understanding of the guidelines of diagnosis and management of sepsis will enable nurses and physicians to combat deaths associated with sepsis. We look forward to analyzing the protocols and procedures laid out in the Surviving Sepsis Campaign of 2016 and apply these findings to hospitals within Saudi Arabia and the world at large. Similarly, the results of our study will allow members of the public to understand the necessary measures that can be taken when a septic emergency occurs at home or outside the vicinity of a hospital. Therefore, this study not only seeks to scrutinize how sepsis is diagnosed and managed but also contributes to reducing the deaths associated with sepsis.
Literature Review
Many studies cite sepsis as the primary cause of deaths experienced in intensive care units. According to Zhang (2015), cases of severe sepsis are continually rising, where the incidences increased from about 143 cases in the year 2000 to approximately 340 cases in every 100,000 people in 2007 in the United States. A similar report by the World Health Organization (WHO) showed that every year, sepsis affects about 30 million people globally, resulting in over 6 million mortalities (Reinhart et al. 2017). With such an alarming rate of deaths caused by sepsis, it is fundamental that in-depth research explores the underlying factors leading to these deaths. Reinhart et al. (2017) observed that septic infections are acquired from both health care facilities and community surroundings. This poses a further risk because hospitals can also be sources for the manifestation of sepsis infection. Waele & Sakr (2019) outline procedures for identifying the sources of sepsis contamination, which involves first identifying the epidemiology of the infection. From their findings, it was discovered that most infections are likely to occur within the intensive care unit rooms and general hospital wards. Hence, extra caution is required when patients are admitted to hospitals over various illnesses since studies indicate that such patients risk getting a septic infection.
Moreover, certain groups of people have a high likelihood of contracting a septic infection. According to a report released by the WHO, the most vulnerable populations comprise of pregnant women, lactating mothers, infants under the age of five years, hospitalized patients, and people who have cancer, HIV/AIDS, and autoimmune syndromes (Singer et al. 2016). Research by Gasim et al. (2016) carried out at one of the intensive care units of Buraidah Central Hospital, Saudi Arabia, identified that the most vulnerable patients of severe septic shock were elderly hospitalized patients with respiratory illnesses. Unfortunately, over 40% of these patients died from shock. Slightly different to the findings by Gasim was the outcome of a study conducted by Aslan et al. (2018). According to their survey of acute kidney injury (AKI), sepsis was the leading factor for kidney failure among critically ill patients admitted in the ICU. Without a doubt, hospitalized patients have a relatively high risk of contracting a septic infection. This calls for scientific researches that can provide reliable diagnostic measures for early identification of the disease and guidelines that minimize the number of deaths experienced in hospitals from sepsis infections.
Third world countries face critical risks of comorbidities and mortalities resulting from sepsis infections. Despite many studies on sepsis having originated from developed countries such as the United States and the United Kingdom, Dagher et al. (2015) examined the prevalence of sepsis in a developing country in the Middle Eastern population and discovered similar facts to those of developed countries. Their study was based in Beirut, Lebanon, where patients in a single tertiary care unit and suffering from septic shock underwent various treatment procedures. Within the first four hours after the attack, a majority of the patients (about 87%) received an antibiotic initiation at the emergency center. Approximately 45% of the patients received treatment from the ICU, and roughly 54% of the other patients were taken to the general practice unit (GPU). Unfortunately, about 31% of the patients succumbed to the septic infections over one month, indicating that developing countries also suffer a high risk of mortalities caused by sepsis contamination (Dagher et al. 2015).
The diagnosis of sepsis is critical because a lack of prompt measures to fight a septic shock often results in adverse effects, where major body organs and cellular tissues become permanently damaged, or the patients die (Fan, Miller, & Remick 2016). However, misdiagnosis is a common phenomenon among sepsis patients due to the concept of Systemic Inflammatory Response Syndrome (SIRS). SIRS and sepsis have similar signs and symptoms, making the diagnostic process, such as a tedious task that can result in the misdiagnosis and prognosis of sepsis. According to Fan, Miller, & Remick (2016), well stipulated clinical laboratory measures are necessary for identifying this life-threatening condition of sepsis and septic shock. One such clinical procedure is the Procalcitonin (PCT) test, which accurately distinguishes between sepsis and SIRS by indicating the level of either an existing infection in the blood or a noninfectious inflammatory response. However, in the absence of an infection, PCT levels may be highly eminent due to other disorders, thus necessitating the use of double or triple concentrations for accuracy.
The lactate procedure is another diagnostic tool that may predict the presence of sepsis infection because lactate levels serve as markers for organ failure during septic shock (Fan, Miller, & Remick 2016). This procedure is approved by the Food and Drug Administration (FDA) as a safe procedure for use in emergency departments or the intensive care units (ICU). Yoo et al. (2019) go ahead to describe that high lactate values indicate a higher risk of mortality or shock. However, elevated lactate levels also appear in acute conditions such as heart attack and seizures (as cited by Fan et al. 2016); thus, the raised levels may give ambiguous interpretations that are not specific to sepsis. A similar procedure is the C Reactive Protein (CRP), which uses serum concentrations to predict acute inflammatory reactions, such as cardiac arrest. When used in the diagnosis and prognosis of sepsis shock, CRP effectively determines a patient’s response to therapy (Gyawali et al. 2015). Other diagnostic procedures for sepsis infection include cytokines, D-Dimer, Proadrenomedullin (ProADM), myocardial concentrates, and the Sequential Organ Failure (SOFA) procedure. The recommendation to physicians in the emergency care departments is to use multiple diagnostic biomarkers in predicting sepsis infection to avoid misdiagnosis (as cited by Weiss et al., 2020).
Chapter 2: Methods
Research design
The design for this study will follow a descriptive comparative research design where we will examine the methods applied by physicians to classify patients in the Intensive Care Units and Emergency Rooms as having severe sepsis. Therefore, we will evaluate the underlying causes of the high mortalities associated with severe sepsis by focusing on the diagnosis and management of sepsis.
Locale of the study
This study will be conducted at the emergency department of a government hospital in Al Madinah in the Kingdom of Saudi Arabia. The hospital is situated in the Medina (Madinah) capital, one of the holiest cities in Islam. The bed capacity of this hospital is about 200, and it offers a wide variety of specialties, such as general surgery, emergency medical services, orthopedic surgery, and neurology.
Participants
The sample for this research will comprise of nurses and physicians working in the casualty department of KFH. The inclusion criteria will specifically focus on services providers currently working in the Emergency Rooms (ER) and the intensive care units (ICU) of the hospital, health practitioners with over six months of work experiences and healthcare workers registered with the Saudi Commission of Healthcare Practitioners. This research will exclude persons currently working outside the ER and ICU units, and nurses and physicians with less than six months of work experience.
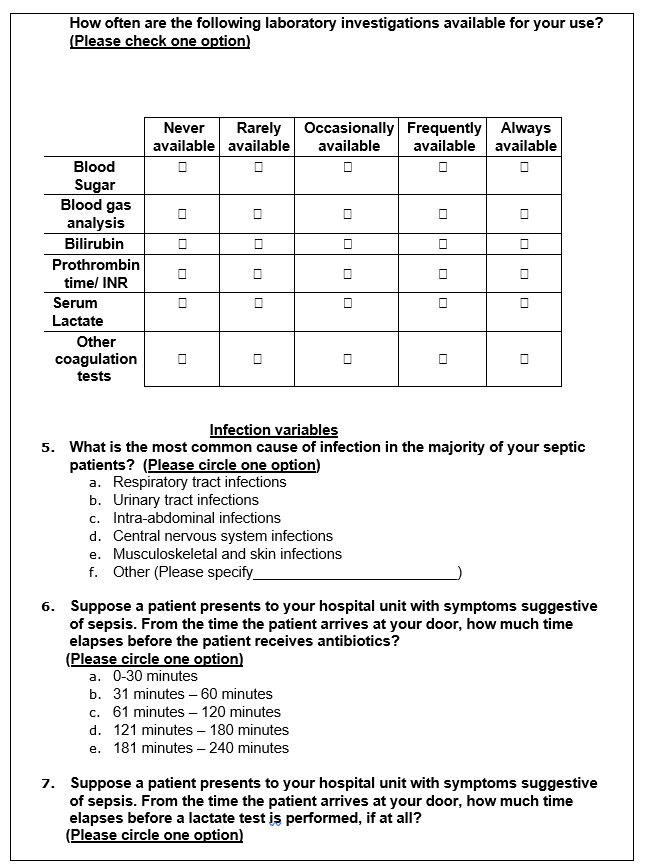
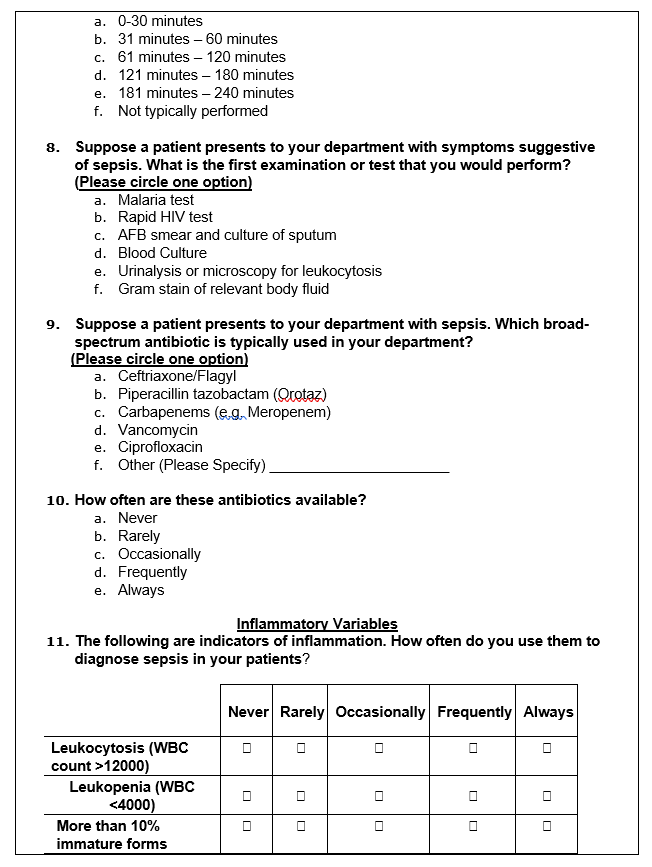
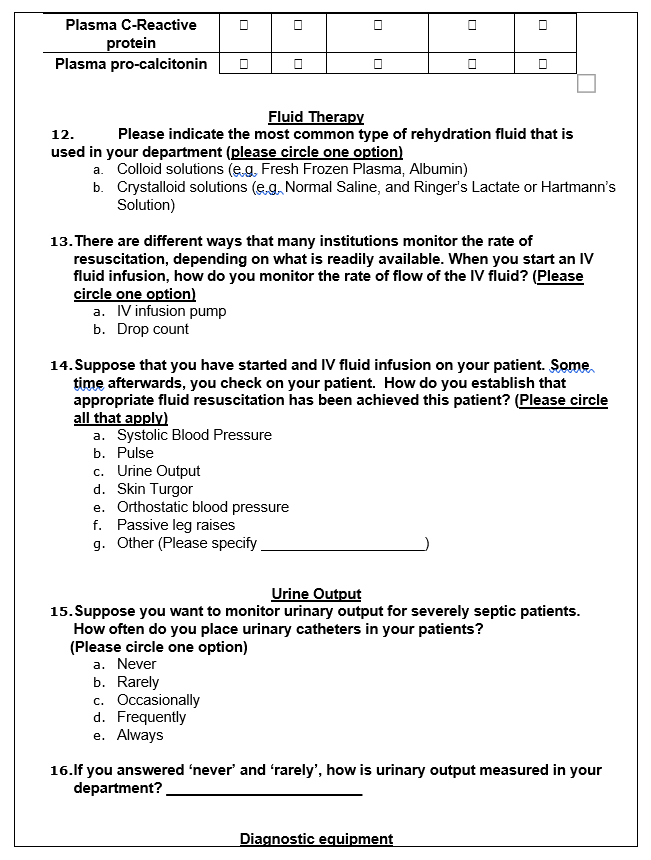
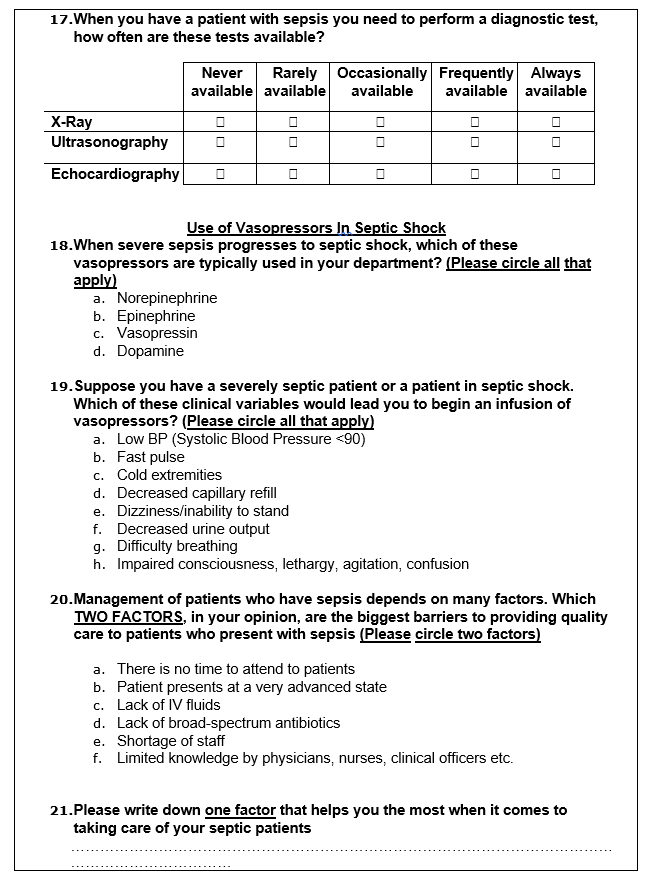
Instrumentation
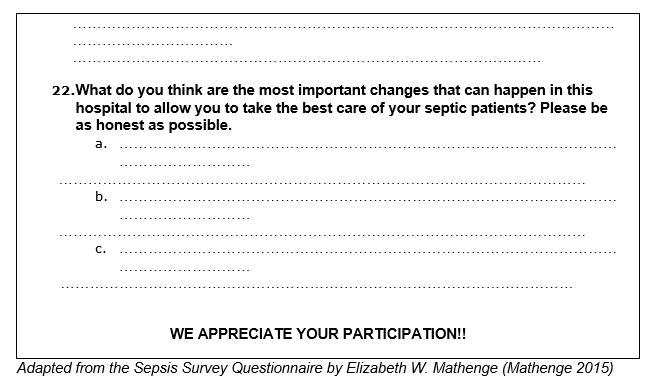
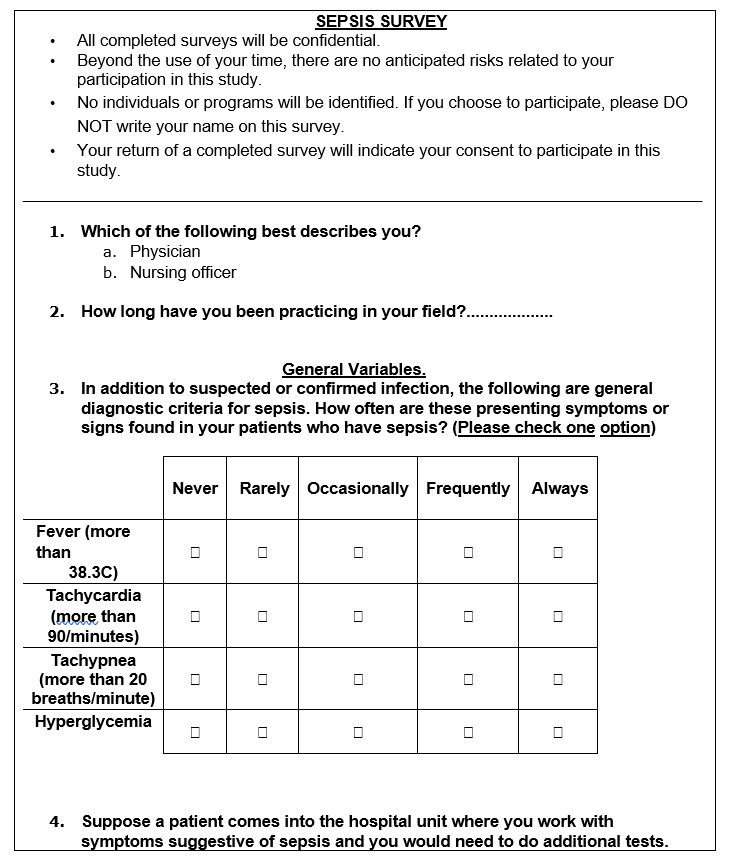
This study will use an adapted questionnaire titled ‘Sepsis Survey’ by Elizabeth Mathenge to collect data on the medical procedures undertaken by nurses and physicians in the management of severe sepsis (Mathenge 2015). The questionnaire will contain 22 questions, both open and closed-ended, that are based on the international guidelines for the management of sepsis and septic shock of the Surviving Sepsis Campaign (SSC) of 2016 (Rhodes et al. 2017).
The variables of interest will cover three significant aspects of septic resuscitation procedures – the general, infection, and inflammatory variables. These variables will be used to determine the diagnostic approaches that physicians use when handling patients with sepsis. Furthermore, the questionnaire will help to determine the equipment and medical interventions most commonly used in managing septic shock. A sample of the questionnaire is given below.
Data gathering procedure
Since this study will largely depend on data sourced from nurses and doctors, an elaborate document detailing the protocol guidelines for this study will aid in securing the approval of the Institutional Review Board (IRB). As such, we will provide a written document that follows the regulations of the Food and Drugs Administration (FDA). Here, the protocol guideline will outline this studies’ objectives, the inclusion and exclusion criteria, the study design, analysis of the results, and data confidentiality.
A reconnaissance or pilot study will also be conducted to identify and obtain consent to interact with hospital staff at the emergency department that will serve as the data collection site. Participants will include all the nurses and doctors in the ER and ICU sections of the hospital under study. However, the pilot study will involve a sample of three healthcare providers, one nurse and two doctors from the emergency department. The aim of the pilot study will be to determine the efficacy of our study design, the reliability of our questionnaires, and the general acceptability of this survey.
Data analysis
Data analysis will involve Microsoft Excel and the Statistical Package for the Social Sciences (SPSS) software, from which descriptive statistics and analysis of variance (ANOVA) will be calculated. One-way ANOVA will determine the differences between groups’ mean scores. On the other hand, pairwise correlations will indicate whether the variations in group scores are significant or not.
The qualitative data from the multiple-choice questions will be coded from the 5-point Likert scale into two categories. The first category will include the first three lower subset of the response options, ‘Never’, ‘Rarely’, and ‘Occasionally’. The second category will encompass the upper subset of the response options, ‘Frequently’ and ‘Always’. The analysis of both the qualitative and quantitative data will contribute to meeting the objectives of this study, which are assessing the knowledge and skills of healthcare professionals in the management of severe sepsis.
Ethical Consideration
No persons or animals will be harmed during this research. All information from KFH records will be treated with the utmost confidentiality and integrity. Before the research is conducted, consent must be given by the IRB to ensure that no breach of conduct is intentionally or otherwise made.
References
Aslan, A., van den Heuvel, M. C., Stegeman, C. A., Popa, E. R., Leliveld, A. M., Molema, G., … & van Meurs, M. (2018). Kidney histopathology in lethal human sepsis. Critical Care, 22(1), 359.
Berg, D., & Gerlach, H. (2018). Recent advances in understanding and managing sepsis. F1000Research, 7.
Dagher, G., Saadeldine, M., Bachir, R., Zebian, D., & Chebl, R. (2015). Descriptive analysis of sepsis in a developing country.
DeVos, E. L. (2018). Updates and Controversies in the Early Management of Sepsis and Septic Shock.
Fan, S. L., Miller, N. S., Lee, J., & Remick, D. G. (2016). Diagnosing sepsis–The role of laboratory medicine. Clinica chimica acta, 460, 203-210.
Gary, T., Mingle, D., & Yenamandra, A. (2016). The evolving definition of sepsis. arXiv preprint arXiv:1609.07214.
Gasim, G. I., Musa, I. R., Yassin, T., Al Shobaili, H. A., & Adam, I. (2016). Sepsis in Buraidah Central Hospital, Qassim, Kingdom of Saudi Arabia. International journal of health sciences, 10(2), 175.
Gyawali, B., Ramakrishna, K., & Dhamoon, A. S. (2019). Sepsis: The evolution in definition, pathophysiology, and management. SAGE open medicine, 7, 2050312119835043.
Mathenge, E. W. (2015). Knowledge, Attitudes and Practices of Sepsis Management at (Doctoral dissertation, Duke University).
Reinhart, K., Daniels, R., Kissoon, N., Machado, F. R., Schachter, R. D., & Finfer, S. (2017). Recognizing sepsis as a global health priority—a WHO resolution. New England Journal of Medicine, 377(5), 414-417.
Rhodes, A., Evans, L. E., Alhazzani, W., Levy, M. M., Antonelli, M., Ferrer, R., … & Rochwerg, B. (2017). Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive care medicine, 43(3), 304-377.
Singer, M., Deutschman, C. S., Seymour, C. W., Shankar-Hari, M., Annane, D., Bauer, M., … & Hotchkiss, R. S. (2016). The third international consensus definitions for sepsis and septic shock (Sepsis-3). Jama, 315(8), 801-810.
Waele, J. J., & Sakr, Y. (2019). How I search for a sepsis source. Critical Care, 23(1), 16-24
Weiss, S. L., Peters, M. J., Alhazzani, W., Agus, M. S., Flori, H. R., Inwald, D. P., … & Brierley, J. (2020). Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Medicine, 46(1), 10-67.
Yoo, J. W., Lee, J. R., Jung, Y. K., Choi, S. H., Son, J. S., Kang, B. J., … & Hong, S. B. (2015). A combination of early warning score and lactate to predict intensive care unit transfer of inpatients with severe sepsis/septic shock. The Korean journal of internal medicine, 30(4), 471.
Zhang, Z. (2015). Biomarkers, diagnosis and management of sepsis-induced acute kidney injury: a narrative review. Heart, lung and vessels, 7(1), 64.