Essay on COVID-19 and Arrhythmia
Number of words: 1019
COVID-19 has been associated with well-documented cardiac problems in people with and without previous cardiovascular disease. Cardiovascular consequences include acute coronary syndrome, heart failure, and myocarditis caused by coronary artery thrombosis or plaque ruptures caused by SARS-CoV-2. Arrhythmias are also a significant problem as evidence grows. According to recent research, around 7% of patients experience palpitations as a presenting symptom. Tajbakhsh et al. (2021) hypothesized that cardiac injury often occurs, particularly in severely sick COVID-19-infected individuals, through various pathways, mostly direct cardiomyocyte damage and systemic inflammation. Arrhythmias have historically been associated with viral infections that cause viral myocarditis, and current anecdotal data suggests that this may also be the case with COVID-19-infected patients.
Arrhythmias and conduction system illness, on the other hand, are not early or frequent signs of COVID-19, and the bulk of symptoms are associated with respiratory system involvement (Babapoor-Farrokhran et al., 2020). While sinus tachycardia has been documented due to the viral infection’s physiological response, arrhythmias other than sinus tachycardia have been found at a substantial incidence in COVID-19 patients. Arrhythmias are a common complication of viral infections, and it seems as though they are generally triggered by viral myocarditis, which affects the cardiac conduction system.
Epidemiology and quality of life of patients
There is substantial evidence that individuals with cardiovascular illness generally and arrhythmias postpone presentation to the health care system. Baldi et al. (2020) reported 9806 instances of Covid-19 in the study region in 2020. Three hundred sixty-two incidents of out-of-hospital cardiac arrest were detected during this period, up from 229 occurrences during the same period in the previous year. As a result, cardiac infarction occurring outside the hospital increased by approximately 60%.
The coronavirus disease (COVID-19) resulted in an outbreak with a high fatality rate spread swiftly worldwide. Immediate cardiac damage characterized by increased troponin, echocardiographic, or electrocardiographic abnormalities were recorded in 12% of first instances in Wuhan, China. Cardiac arrests and arrhythmias, according to Bhatla et al. (2020), are more than likely the result of systemic disease rather than the direct result of COVID-19 infection. There were nine cardiac arrests, 25 incident AF episodes, nine clinically meaningful bradyarrhythmias, and 10 NSVTs among 700 individuals. As seen in the figure below, all cardiac arrests happened in patients hospitalized in the intensive care unit.
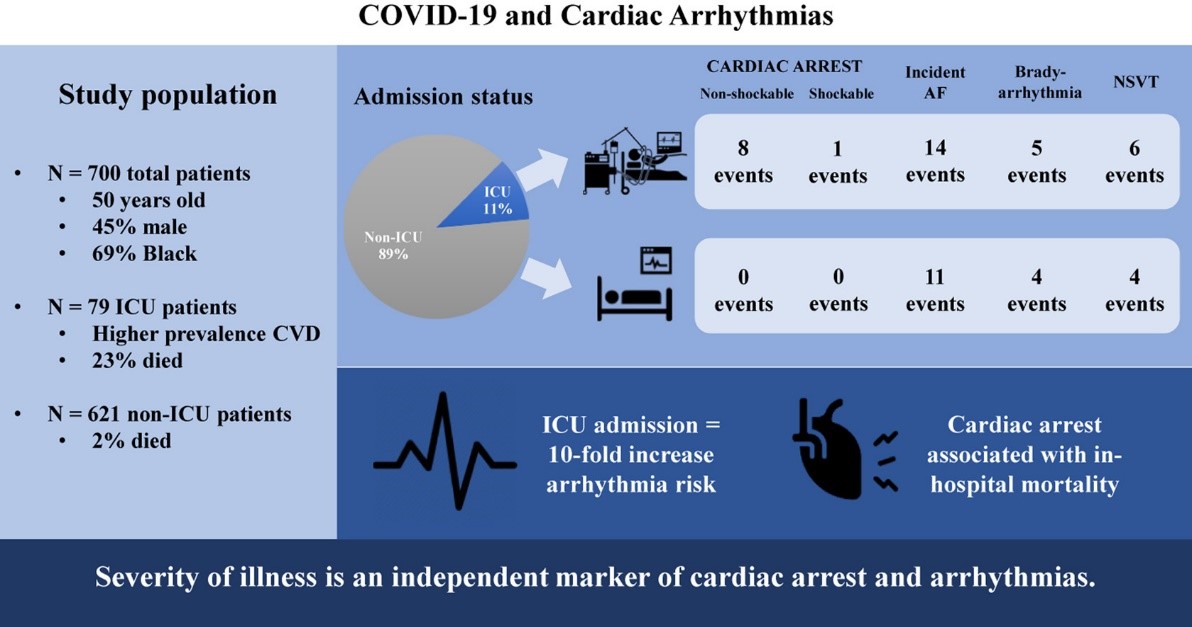
Figure 1: Covid-19 on Arrhythmias (Bhatla et al., 2020)
The examination of the causes of mortality in COVID-19 patients indicated that about 40% of fatalities occurred owing to heart failure and myocardial injury (Kochi et al., 2020). Another research conducted in China discovered that 17.3 percent of COVID-19 patients hospitalized with high troponin had ventricular tachycardia (VT) or ventricular fibrillation (VF). COVID-19, commonly believed, can induce cardiac damage through myocarditis, resulting in heart failure and increasing the risk of VT or VF. Additionally, increased sympathetic tone and cytokine storm have been proposed as possible causes of ventricular arrhythmias (VA). While VT or VF was common consequences in individuals with COVID-19 in China, the exact prevalence and features of cardiac arrhythmias in other world areas remain unclear.
Management and Treatment of COVID-19 Linked to Arrhythmia.
Cardiac arrhythmias are a recognized consequence of COVID-19 infection that may remain long after the infection has been resolved. Cardiac arrhythmias such as ventricular tachycardia, total heart block, supraventricular tachycardia, and atrial fibrillation occur in individuals who are infected with COVID-19, recovering from it, or who have recovered from it. Clinicians should be on the lookout for possible rhythm abnormalities in patients receiving COVID-19. Around 4% of COVID-19 patients have a history of cardiac arrhythmias and may be more prone to developing further rhythm problems (Wang et al., 2020). As a result, it is necessary to obtain critical clinical information, such as a history of arrhythmias, unexplained syncope, family history of sudden cardiac death, and detailed medication history, particularly medications that can cause electrocardiographic QT prolongation, as well as baseline electrocardiograms. To avoid adverse clinical outcomes in patients with underlying cardiovascular illness, it is critical to monitor their ECG anomalies and the possible risk of cardiac arrhythmias. A baseline assessment is required to screen individuals hospitalized or at an increased risk of cardiac arrhythmias. If COVID-19 patients show dizziness, palpitation, or even unexplained syncope, cardiac arrhythmia monitoring should be undertaken. If the baseline ECG indicates a somewhat prolonged QTc, medication and electrolyte optimization may allow for treatment. If the QTc is significantly extended, medicines that prolong it should be avoided; nevertheless, professional advice may allow administration with mitigating measures.
In conclusion, although COVID-19 outbreaks pose a concern to public health, the extra-pulmonary symptoms and their long-term implications are frequently neglected. According to previous research, cardiac arrhythmias are a frequent consequence of COVID-19, which can be fatal in certain cases. It is proposed that front-line physicians monitor heart rhythm as part of standard treatment, and the data may provide light on whether arrhythmic problems associated with COVID-19 are a significant predictor of poor outcomes. Early treatment and diagnosis are critical for reducing mortality.
References
Babapoor-Farrokhran, S., Rasekhi, R. T., Gill, D., Babapoor, S., & Amanullah, A. (2020). Arrhythmia in COVID-19. SN Comprehensive Clinical Medicine, 1-6. DOI https://doi.org/10.1007/s42399-020-00454-2
Baldi, E., Sechi, G. M., Mare, C., Canevari, F., Brancaglione, A., Primi, R., … & Savastano, S. (2020). Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. New England Journal of Medicine, 383(5), 496-498. https://doi.org/10.1056/NEJMc2010418
Bhatla, A., Mayer, M. M., Adusumalli, S., Hyman, M. C., Oh, E., Tierney, A., … & Deo, R. (2020). COVID-19 and cardiac arrhythmias. Heart rhythm, 17(9), 1439-1444.
Kochi, A. N., Tagliari, A. P., Forleo, G. B., Fassini, G. M., & Tondo, C. (2020). Cardiac and arrhythmic complications in patients with COVID‐19. Journal of cardiovascular electrophysiology, 31(5), 1003-1008.
Wang, Y., Wang, Z., Tse, G., Zhang, L., Wan, E. Y., Guo, Y., … & Liu, T. (2020). Cardiac arrhythmias in patients with COVID‐19. Journal of arrhythmia, 36(5), 827-836.