Essay on Chemical Warfare Agents
Number of words: 3261
Introduction
Chemical weapons were first deployed and used in World War I and II. Chemicals weapons are particularly effective in destroying enemies during war. Presently, there are over 50 different types of chemicals developed to be primarily used as chemical weapons (Bentley, 2018). As multiple states began using chemical weapons, this resulted in the banning of some of them (Bentley, 2018). There are four main types of chemical weapons, namely incapacitants, choking agents, blistering agents and blood agents. Chemical weapons affect the human body by causing the build-up of fluids, impeding with the transfer of oxygen, paralysis, organ failure and in some cases, death. This essay will provide a robust assessment of the mechanism of working of the chemical agents and the available treatment options in case of exposure to the agents.
Incapacitants
Chemical warfare agents and specifically Incapacitants usually paralyse, disorient or incapacitate humans. There have been experiments on a wide range of Incapacitants such as LSD (lysergic acid diethylamide), methaqualone, mescaline and BZ (3-quinuclidinyl benzilate). The experiments have shown that those weapons are not primarily designed not to kill but instead to incapacitate and disorient opponents (Gupta, 2015). However, if the Incapacitants are taken in excessive doses, they might result in death or permanent injuries. In particular, BZ and LSD, when taken in high doses, usually attack the nervous system and adversely affect the mental processes; for instance, psychotic thinking and hallucinations (Gupta, 2015; Haines & Fox, 2014). Furthermore, some of the Incapacitants might cause individuals to be slow to respond or sleep.
Mechanism of working
The primary mode of functioning of the incapacitants is impeding with the effective and efficient function of the CNS (Central Nervous System). Specifically, the incapacitants usually interfere with the cholinergic transmission of cellular messages at the muscarinic sites and in particular, in the spinal cord, brain and the peripheral nervous system (Price, 2018; Spiers, 2016). In particular, the incapacitants usually decrease the effective concentration of acetylcholine (ACh) at the mAChR (muscarinic receptor) (Sydnes, 2013). This results in limited ACh getting to the end organs (Ganesan et al., 2010). Ultimately, this results in the under stimulation of exocrine glands and smooth muscles (end organs) (Ganesan et al., 2010). However, the incapacitants do not have any direct effect on the skeletal muscle (Marrs et al., 2007).
Further, it should get noted that the impacts of incapacitants on the heart rate largely depends on their compounds. For instance, atropine initially causes brief tachycardia that in the long term changes into pronounced tachycardia (Marrs et al., 2007). On the other hand, BZ initially causes tachycardia that lasts for 1-2 days. In the long term, BZ causes mild bradycardia (Marrs et al., 2007).
Treatment options
For most victims of the exposure to incapacitants, all that is required is symptomatic treatment. As incapacitants increase the risk of the victims developing stroke, health care providers and first responders should ensure that they remove the clothes of the casualties and place them in a space where there is the free circulation of air (Moshiri et al., 2012). In the case of victims, who appear to be in considerable danger, physostigmine needs to get administered to them as it is a good antidote for some of the incapacitants such as BZ (Moshiri et al., 2012).
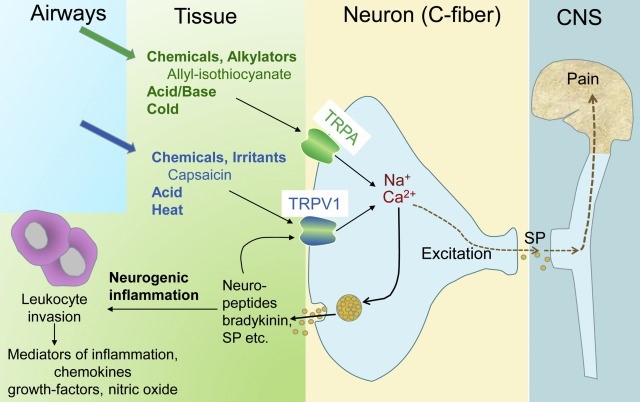
Figure 1.0 Targets of Chemical Weapons (Schwenk, 2018)
Nerve agents
Additionally, chemical warfare agents and in particular, nerve agents often adversely affect the transmission of impulses and signals in the nervous system (Krutzsch et al., 2014). Nerve agents often result in blurred vision, convulsions, defaecation, blocking of bronchial passages with mucus, profuse sweating, paralysis and respiratory failure (Krutzsch et al., 2014). Respiratory exposure to nerve agents often leads to asphyxia and subsequently, death. Excellent defence against nerve agents often requires robust protective overgarments and skin-tight masks (Krutzsch et al., 2014). Some of the examples of nerve agents include Soman, Sarin and Vx. Soman and Sarin were both invented in Germany in 1938 and 1944, respectively (Patocka, 2016). VX, on the other hand, was invented in a British government institution (Pitschmann, 2014).
Figure 2.0 How Nerve Agents work (Alchetron, 2018)
Mechanism of Working
As stated previously, the primary mode of working of the nerve agents is through the disruption of the central nervous system (CNS) communicating channels, which results in the complete shutdown of the body’s nervous system (Seto, 2020). Cellular messaging is one of the essential elements of the nervous system. The body achieves cellular messaging by transmitting electrical impulses along the nerves (Seto, 2020). With the aid of neurotransmitters, the electrical impulses pass from one neuron to another (Seto, 2020; Black, 2016). The most common neurotransmitter in the ACh that transmits the important electrical impulses through the neural network. It is worth noting that ACh also mediates muscle contact (Black, 2016). After ACh has performed its function of transmitting cellular messages, the body destroys it using AChE (acetylcholinesterase). The destruction of ACh is particularly crucial as it averts the overstimulation of the nervous system (Black, 2016; Worek et al., 2016).
Ordinarily, organophosphate nerve agents disrupt the body’s natural destruction of the ACh. In particular, the organophosphate nerve agents attach themselves to particular sites of the AChE, therefore impeding with its normal functioning (Lukey et al., 2019). As a result, this leads to the toxic build-up of ACh, which leads to the overstimulation of the nervous system (Lukey et al., 2019). After one has been exposed to the nerve agents, the build-up of the ACh in the body results in the loss of muscular function (Lukey et al., 2019). Subsequently, this leads to respiratory arrest, paralysis, convulsions, drooling, and constriction of pupils. If the victim does not obtain treatment, he/she will inevitably die (Salem et al., 2019).
Treatment Options
The treatment to the exposure of the nerve agents entails reversing the toxic accumulation of ACh in the body. Usually, the victims get given oxime drugs to break down the bond connecting AChE and the nerve agent. As a result, this regenerates AChE for routine use by the body (Salem et al., 2019). It should get noted that speed is essential when administering the oxime drugs to a victim of exposure to the nerve agents (Ballantyne & Marrs, 2017). Undoubtedly, this is because the bond between the nerve agent and AChE strengthens (ages) over time (Ballantyne & Marrs, 2017). A stronger bond between AChE and the nerve agents renders the oxime drugs ineffective (Guidoti & Trifiro, 2016).
Although in healthy individuals, atropine is poisonous as it disrupts communication between cells; this is not the case for individuals poisoned with a nerve agent (Guidoti & Trifiro, 2016). Atropine functions by blocking ACh receptors and therefore inhibiting cellular messaging (Guidoti & Trifiro, 2016). Atropine often blocks the ACh receptors at the muscarinic sites (Guidoti & Trifiro, 2016). As a result, this minimises the adverse impacts of excessive ACh on the receptor sides. In instances, where there is rapid ageing between the nerve agents and the AChE, prophylactic agents and components such as pyridostigmine should be used (Thiermann et al., 2017). The prophylactic agents prevent the nerve agent from attaching itself to the AChE (Mangerich & Esser, 2014). However, the use of prophylactic agents does not negate the need to receive treatment using atropine and oxime derivatives (Mangerich & Esser, 2014).
Blistering agents
Furthermore, some of the chemical weapons, and in particular blistering agents often cause the corrosion of skin and the burning of eyes, lungs and mouth. Blistering agents first got developed and used in World War I. The type of blistering agent that was used in World War I mustard gas (sulphur mustard). The blistering agents are often delivered in vapour or liquid form (Trapp, 2017). The effects of blistering agents on the human body often depend on the level of exposure. In cases of exposure to high concentrations of blistering agents, the effects of the blistering agents tend to be immediate (Trapp, 2017). Despite being very lethal at high concentration, blistering agents rarely result in death. Some of the blistering agents that are commonly used nowadays include lewisite, phosgene oxime, nitrogen mustard, and sulphur mustard (Singh et al., 2010). The best protection mechanism against blistering agents is wearing protective over garments or gas masks (Singh et al., 2010).
Mechanism of Working
Sulfur mustard (SM) which is the most common blistering agent is a bi-functional alkylating agent, which contains two reactive Chloroethyl functions. It functions by binding itself to a wide range of molecules that are important for the biological functioning of the body (Ghabili et al., 2011). Some of the molecules, which SM binds onto, include nucleic acids and proteins (Ghabili et al., 2011). The intermediary of the binding of SM into molecules such as proteins and nucleic acids has two chemically active regions which, when attached to the DNA, results in cross-linking and eventually cell death (Ghabili et al., 2011).
In liquid format, SM appears as an oily and dark yellow component with a characteristic pungent smell. Similarly, SM appears as vapour in higher-ambient temperatures (Ghabili et al., 2011). Since SM has a higher density than air, its residual vapour collects in low-lying areas for extended periods (Shakarjian et al., 2010). Nonetheless, it should get noted that the exact mechanism of working of the blistering agents is not yet well known.
Treatment options
Arguably, since patients who have been exposed to blistering agents such as SM may contaminate their environment, health care practitioners and first responders should ensure that they don personal protective equipment and minimise contact with the patient (Shakarjian et al., 2010). The prehospital considerations when attending to these patients include rapid de-contamination, fast removal from the hazardous area and rapid transportation to the hospital settings (Shakarjian et al., 2010). However, it should get noted that there is not any widely recognised treatment framework for patients who have been exposed to SM (Sezigen et al., 2019). Nonetheless, medical management should typically involve rapid de-contamination using sufficient amounts of water and soap (Sezigen et al., 2019). Subsequently, the victim should be offered supportive care that generally encompasses basic burn dressing, infection prevention, analgesia, respiratory support and the administration of fluids. In instances, where the victim sustains large blisters, it is advisable to lance and debride them so that they can heal at a relatively faster rate (Sezigen et al., 2019). It may also be necessary to administer GM-CSF or Sodium thio-sulphate to the victims of the blistering agents (Sezigen et al., 2019).
Choking agents
Lastly, chemical weapons, such as choking agents, usually cause choking. Choking agents were first used in World War I by the Allied forces and Germany. In particular, the Germans releases chlorine gas from multiple cylinders. As World War, I progressed the different parties in the war started using other choking agents such as chloropicrin, phosgene, ethyldichlorasine, diphosgene and perfluoroisoboxylene (Trapp, 2017). When deployed, choking agents may result in disastrous outcomes; for instance, 80% of the deaths in World War I can be attributed to phosgene (Trapp, 2017). Choking agents usually get delivered in the form of gas clouds to the targeted body areas. When inhaled, the choking agents cause the build-up of fluids in the body.
Mechanism of working
The mechanism and mode of working of the choking agents depend significantly on their nature and form. Notably, choking agents that are highly soluble in aqueous solutions and highly reactive (centrally-acting agents) predominantly acts in the central compartment of the respiratory tract (Zellner & Eyer, 2020). Some examples of the centrally acting irritants include ammonia, mustard, sulphur and hydrochloric acids (Zellner & Eyer, 2020). These centrally-acting irritants result in considerable irritation of the epithelial cells that line the upper airway (Zellner & Eyer, 2020).
On the other hand, choking agents that are insoluble and not highly reactive (peripherally acting agents) such as nitrogen oxides, phosgene, and PFIB, penetrate to the level of bronchioles and the alveoli (Zellner & Eyer, 2020). In the bronchioles and the alveoli, these choking agents typically undergo acylation reactions. In most cases, these agents are consumed in the bronchioles and alveoli, causing substantial damage that may lead to pulmonary oedema (Anderson, 2012). The acute lung injury caused by these choking agents often involves a permeability defect in the alveolar-capillary membrane (blood-air barrier). Nevertheless, the exact mechanism of toxicity largely remains unknown (Anderson, 2012).
Usually, lymphatic drainage from the parenchyma compensates the leakage of fluids from the capillaries to the pulmonary interstitium (Anderson, 2012). However, in the long run, the standard drainage mechanisms get overwhelmed by the continued fluid leakage. Further, after a latent period ranging between 20 minutes to 24 hours (which is highly dependent on the exposed dose) fluid leakage into the pulmonary interstitium reduces compliance and therefore results in the stiff lung (Anderson, 2012). Additionally, it increases complaints of dyspnoea, shortness of breath and tight chest. Ultimately, the fluid invades the alveoli resulting in pulmonary oedema that is clinically evident (Anderson, 2012).
Moreover, it should get noted that the distinction between centrally and peripherally acting agents is relaxed. Therefore, this means that after exposure to high concentrations of the centrally-acting choking agents, some of them may pass into the peripheral lung and cause pulmonary oedema (Anderson, 2012). Similarly, after exposure to high concentrations of peripherally-acting agents, they can release sufficient hydrochloric acid which that substantial damage to the epithelial cells that line the upper airway and irritation of the central airway (Anderson, 2012).
Treatment Option
Arguably, the treatment of exposure to the choking agents first involves ending the exposure. Typically, this will be achieved by physically removing the patient from the hazardous environment. The exposure can also be ended by covering the victim with an appropriately fitting respirator (Anderson, 2012). Further, it is necessary to enforce rest and warmth to an individual who has been exposed to the choking agents. Usually, the choking agents often result in coughing and tightness of the chest (Anderson, 2012). In instances, where the victim exhibits orthopnoea or dyspnoea, he/she should get evacuated in a semi-sitting position.
Besides, as stated previously, pulmonary oedema will always follow the exposure to high concentrations of the choking agents (Anderson, 2012). There to mitigate the risk of pulmonary oedema, it is necessary to administer to the victim corticosteroids. Although corticosteroids are highly recommended, there is no proof of their benefits (Kuca & Pohanka, 2010). Initiating the steroid treatment within a short period after the exposure to the choking agents has been shown to minimise the severity of pulmonary oedema (Kuca & Pohanka, 2010). The steroid treatment should ideally get started within 15 minutes after the exposure to the choking agents. The steroid treatment should involve two inhalation regimes; dexamethasone and either beclomethasone or betamethasone (Kuca & Pohanka, 2010). Besides, the steroids should be administered in high doses through inhalation. In severe cases, an injection of the steroids should be administered (Kuca & Pohanka, 2010).
Conclusion
To sum it up, the essay has presented a robust assessment of the effects of chemical warfare agents on the human body. In particular, the essay has shown that there is a wide range of chemical weapons such as choking, blistering, blood and nerve agents. All these have different working mechanisms. The paper has also provided possible treatment options in case of exposure to the chemical agents.
References
Alchetron, 2018. Nerve agent – Alchetron, The Free Social Encyclopedia. [online] Alchetron.com. Available at: <https://alchetron.com/Nerve-agent> [Accessed 25 Nov. 2020].
Anderson, P.D., 2012. Emergency management of chemical weapons injuries. Journal of pharmacy practice, 25(1), pp.61-68.
Ballantyne, B. and Marrs, T.C., 2017. Clinical and experimental toxicology of organophosphates and carbamates. Elsevier.
Bentley, M., 2018. Syria and the chemical weapons taboo: Exploiting the forbidden.
Black, R., 2016. Development, historical use and properties of chemical warfare agents.
Ganesan, K., Raza, S.K. and Vijayaraghavan, R., 2010. Chemical warfare agents. Journal of pharmacy and bioallied sciences, 2(3), p.166.
Ghabili, K., Agutter, P.S., Ghanei, M., Ansarin, K., Panahi, Y. and Shoja, M.M., 2011. Sulfur mustard toxicity: history, chemistry, pharmacokinetics, and pharmacodynamics. Critical reviews in toxicology, 41(5), pp.384-403.
Guidotti, M. and Trifirò, F., 2016. Chemical risk and chemical warfare agents: science and technology against humankind. Toxicological & Environmental Chemistry, 98(9), pp.1018-1025.
Gupta, R.C. ed., 2015. Handbook of toxicology of chemical warfare agents. Academic Press.
Haines, D.D. and Fox, S.C., 2014. Acute and long-term impact of chemical weapons: lessons from the Iran-Iraq war. Forensic Sci Rev, 26(2), pp.97-114.
Krutzsch, W., Myjer, E. and Trapp, R. eds., 2014. The chemical weapons convention: a commentary. OUP Oxford.
Kuča, K. and Pohanka, M., 2010. Chemical warfare agents. In Molecular, Clinical and Environmental Toxicology (pp. 543-558). Birkhäuser Basel.
Lukey, B.J., Romano Jr, J.A. and Salem, H. eds., 2019. Chemical Warfare Agents: Biomedical and Psychological Effects, Medical Countermeasures, and Emergency Response. CRC Press.
Mangerich, A. and Esser, C., 2014. Chemical warfare in the First World War: reflections 100 years later. Archives of Toxicology, 88(11), pp.1909-1911.
Marrs, T.T., Maynard, R.L. and Sidell, F. eds., 2007. Chemical warfare agents: toxicology and treatment. John Wiley & Sons.
Moshiri, M., Darchini-Maragheh, E. and Balali-Mood, M., 2012. Advances in toxicology and medical treatment of chemical warfare nerve agents. DARU Journal of Pharmaceutical Sciences, 20(1), p.81.
Muhammad, B.A., 2016. Effects of chemical weapons on cancer development in human. Kurdistan Journal of Applied Research, 1(1), pp.50-60.
Patocka, J., 2016. Syria conflict and chemical weapons: what is the reality. Mil Med Sci Lett, 85, pp.39-43.
Pitschmann, V., 2014. Overall view of chemical and biochemical weapons. Toxins, 6(6), pp.1761-1784.
Price, R.M., 2018. The chemical weapons taboo. Cornell University Press.
Salem, H., Ternay Jr, A.L. and Smart, J.K., 2019. Brief history and use of chemical warfare agents in warfare and terrorism. Chemical Warfare Agents, Chemistry, Pharmacology, Toxicology, and Therapeutics, pp.1-20.
Seto, Y., 2020. On-site detection of chemical warfare agents. In Handbook of Toxicology of Chemical Warfare Agents (pp. 983-1003). Academic Press
Sezigen, S., Ivelik, K., Ortatatli, M., Almacioglu, M., Demirkasimoglu, M., Eyison, R.K., Kunak, Z.I. and Kenar, L., 2019. Victims of chemical terrorism, a family of four who were exposed to sulfur mustard. Toxicology letters, 303, pp.9-15.
Shakarjian, M.P., Heck, D.E., Gray, J.P., Sinko, P.J., Gordon, M.K., Casillas, R.P., Heindel, N.D., Gerecke, D.R., Laskin, D.L. and Laskin, J.D., 2010. Mechanisms mediating the vesicant actions of sulfur mustard after cutaneous exposure. Toxicological sciences, 114(1), pp.5-19.
Singh, B., Prasad, G.K., Pandey, K.S., Danikhel, R.K. and Vijayaraghavan, R., 2010. Decontamination of chemical warfare agents. Defence science journal, 60(4), p.428.
Spiers, E.M., 2016. Chemical warfare. Springer.
Sydnes, L.K., 2013. Update the Chemical Weapons Convention. Nature, 496(7443), pp.25-26.
Thiermann, H., Worek, F. and Kehe, K., 2013. Limitations and challenges in treatment of acute chemical warfare agent poisoning. Chemico-biological interactions, 206(3), pp.435-443.
Trapp, R., 2017. The use of chemical weapons in Syria: Implications and consequences. In One Hundred Years of Chemical Warfare: Research, Deployment, Consequences (pp. 363-375). Springer, Cham.
Worek, F., Jenner, J. and Thiermann, H. eds., 2016. Chemical warfare toxicology: volume 2: management of poisoning. Royal Society of Chemistry.
Zellner, T. and Eyer, F., 2020. Choking agents and chlorine gas–History, pathophysiology, clinical effects and treatment. Toxicology letters, 320, pp.73-79.