Essay on the Significance of Evidence-Based Practice for Sports Therapy
Number of words: 3137
Introduction
Evidence based practice (EBP) is a concept which exists in many industries and disciplines, although this assignment specifically covers its use in Sports Therapy. To commence this assignment, clarifying a more general definition of EBP seems apt, prior to venturing into the specifics about how it is relevant to Sports Therapy and all the practices that exist in this. HHS (2014) defines EBP concisely as applying the best available research results to inform making decisions in health care. This definition also acknowledges the extent to which theory and other variables are applicable to EBP, such as taking into account patient preferences over their treatment (providing that they have the necessary cognitive capacity to be trusted to make such decisions).
The function of this essay is to widely state the barriers which may be resultant from EBP in Sports Therapy and also clarify the significance of it towards Sports Therapy and to what extent it is relevant to practice. It will consult a large body of literature, with a sustained critical appraisal of each piece of literature and reference evident to ensure that the essay attains some credibility in the points that it makes. Furthermore, the essay will also come to an ultimate conclusion on what actually constitutes exemplary EBP in Sports Therapy, the steps which are taken to achieve it, the different forms of research (such as Qualitative and Quantitative) which need to be instituted in order to undertake it and also looking at the Hierarchy of Research Evidence, something which is central to EBP, whilst simultaneously discerning what the significance of EBP is to Sports Therapy and the challenges which surround its implementation (such as lack of knowledge and expertise and client mistrust).
What are the steps of Evidence Based Practice?
EBP is a complex phenomenon, with several perspectives existing on how best to implement it. There are numerous perspectives which exist on its optimal method of integration, but prior to entering into a discussion on what constitutes the best manner of implementing EBP, it seems advisable to communicate a more in-depth definition of it than was expressed in the introduction, assisted by diagrams and other such entities. Although EBP is assumed to have a series of variables and underlying items which constitute it, it mainly only exists of three things, which are noted in the diagram below:
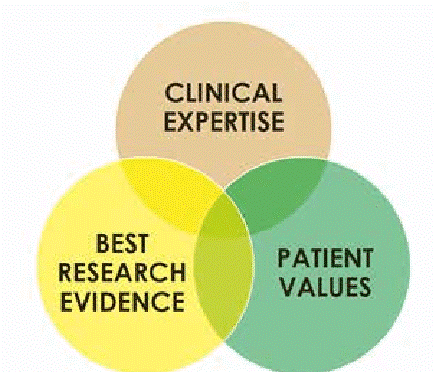
Rubin and Parrish (2007) note that EBP is composed of the three variables of clinical expertise, patient values (or preferences) and best research evidence, all of which can have some bearing on how sports therapists use it in their work and also on the effectiveness of it. The clinical expertise of staff may be central to its success, as is the best research evidence used (although it is debatable as to what constitutes ‘best research evidence’) and the patient’s values or preferences may also have some effect on the efficacy of EBP. Manske and Lehecka (2012) note that the attitude of patients can actually be a barrier towards EBP being successful: for example, if EBP is perceived to be a new and unconventional approach which deviates from the norm (although it is informed by several decades of empirical research and practice), then patients may become reluctant and sceptical towards its advantages and actually be quite disparaging towards it and be non-compliant with the therapy which the sports therapist is providing. It seems similar to the analogy of a teacher in a classroom: arguably, if the pupils are unresponsive then this may limit the ability of them to learn, in a similar manner to if the patient is unresponsive to EBP, this could deprive them of the abundant benefits it can provide.
Supplementing this point, there seems to be a sequential process which therapists must progress through in order to achieve successful implementation of EBP. Strauss et al. (2005) outline the following model which illustrates the processes which one must go through in order for EBP to be successful:
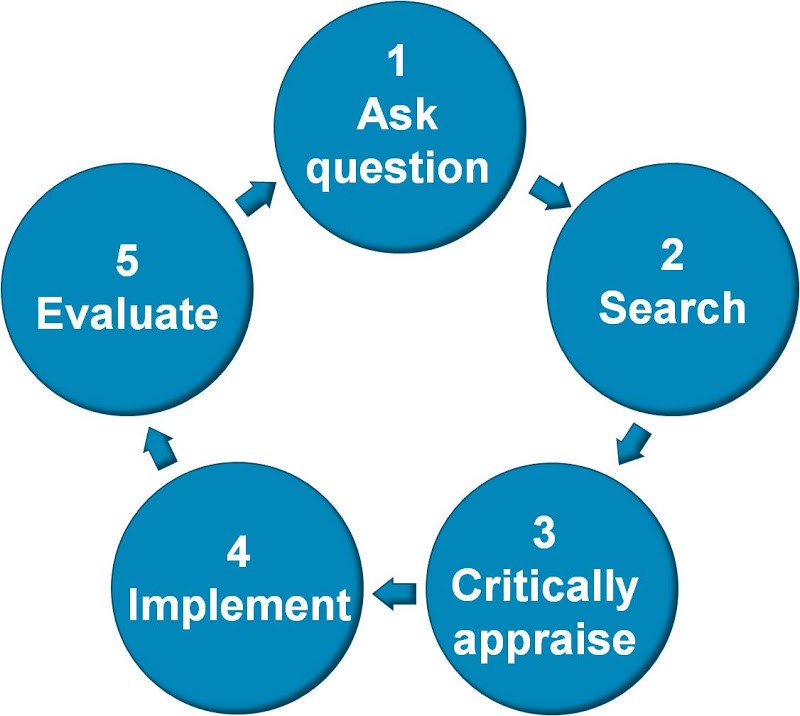
This demonstrates the cyclical nature of EBP and that it is certain that a therapist (or health professional) will iterate through these stages in order to continuously refine and improve their practice, something which needs to be present in order for EBP to be successful: continual renewal and enhancement of one’s practice.
Rubin (2012) converses about the initial step of integrating EBP: asking the question, which involves the conversion of the information which is on hand about the illness or affliction into an answerable question. The information which is available about the illness or injury is known as the aetiology of that illness and forms an essential component of the integration of EBP (Guyatt et al., 2008) as one must understand the determinants behind the illness to be aware of the mechanisms of how to treat it. Then, Rubin (2012) elaborates that one must be mindful of the literature which exists which pertains to that illness or injury, in other words the evidence base. Then, this information is critically appraised, in order to sort between the information which is valid and reputable and that which is irrelevant and unreliable.
As well as sorting between the content of the literature, a kind of grading exists with which to sort the validity and reference of the literature, which is known as the Hierarchy of Evidence. This is known as a method for ranking the accuracy and reliability of numerous qualitative and quantitative research approaches (Polit and Beck, 2014). It is a useful tool which has been prevalently used all across healthcare and has significant implications in assessing the evidence which is collected during the assessment phase of EBP. A diagrammatic representation of it is depicted below:

The Hierarchy of Evidence is something which is well-renowned in several disciplines, particularly Healthcare. As is to be expected, items at the bottom of the pyramid are less reliable than those towards the top. It is also worth noting that the Hierarchy of Evidence is not identical and uniform: several versions of it exist, although Ho et al. (2008) question whether the hierarchy is too rigid and whether the existence of several versions is useful, rather than contributing to ambiguity.
There are several research designs in the Hierarchy of Evidence, but they can be dichotomised into qualitative and quantitative research approaches, which are both common methods of research design. Babbie (2010) defines quantitative research as collecting numerical and statistical evidence, normally on a series of pre-defined scales and which is entirely objective and is supposedly unaffected by subjectivity. He also reports that qualitative research is antithetical to quantitative research in that it is the collection of textual, rather than numerical responses and individual’s experiences of phenomenon. Some of the items in the Hierarchy of Evidence are qualitative (i.e. case reports, ideas and editorials, while some are solely quantitative (cohort studies). It could be argued that some of the study designs mentioned in the Hierarchy of Evidence could be both qualitative and quantitative (systematic reviews and Meta-Analyses), which explains their inclusion at the apex of the pyramid in being the most accurate of the research designs on offer (Muijis, 2010).
It is hard to discern between quantitative and qualitative research as both have their respective advantages and disadvantages, qualitative research is certainly more flexible than quantitative research, but lacks the rigour and definitive nature which qualitative research possesses (Denscombe, 2010). Denscombe (2010) also elaborates that quantitative research and qualitative research are better when combined, rather than being disjoint and separate from each other. This finding is concurrent with the notion of a mixed methods paradigm, which specifies using both quantitative and qualitative data collection and research methods in the context of a study (Denzin, 2009).
After this stage, it is then necessary to implement the information from the research which has been undertaken in the third stage of implementing EBP (‘critically appraise’, as seen in Strauss et al. 2005, which was referenced earlier in the assignment) with the clinical expertise which is at the professional’s disposal and also by taking the situation of the patient into account (such as their circumstances, cognitive capacity and also the severity of their illness or injury) in providing care to the patient. This is reminiscent of person-centred care which exists across many disciplines in healthcare, including nursing and Sports Therapy (Price, 2006). The final stage involves assessing and appraising care as per the remit of looking into the model and scrutinising it to inform a gradual period of refinement and improvement, which is something which is essential to become a reflective practitioner, regardless of the industry which you work in (Schön, 1991).
The significance of EBP to Sports Therapy and the barriers towards implementing it
The issue of EBP has been covered extensively in this assignment so far and has been consulted from numerous angles; however, it has not yet been related to Sports Therapy, which is the mandate of this assignment. It seems to be irrefutable that EBP is crucial to practice in healthcare professions, but the reasons for why it is particularly significant in Sports Therapy need to be clarified for the essay to satisfy the briefs of the question.
Manske and Lehecka (2012) articulate the importance of it to Sports Therapy as an industry in particular: it can have an innumerable amount of advantages: the first being that it can improve the health and well-being of clients (if contemporary and recent/up-to-date theory is applied), promote positive outcomes in their health and also help to challenge the pre-conceived ideas and beliefs which patients may have towards the treatment they receive.
Di Leva (2010) notes that education and Sports Therapy are concomitant with each other: i.e. they are hand in hand, explained at a rudimentary level. EBP is undeniably a form of education as professionals are actively consulting a wide evidence base of literature to inform their care and it could allow them to come across some new information which they did not previously have access to. This is undoubtedly a form of education as the sports therapists are arguably conducting research which is external to their role and shows commendable dedication and work to achieve their goals. The World Health Organisation (WHO) recognises that the traditional and philosophical function of Sports Therapy is to focus on letting the body heal itself naturally, without any interference from any other entities (such as surgical or therapeutic procedures and interventions) and to allow the promotion of healthy lifestyles and diets in patients, with an emphasis on empowering them to take control of their health.
However, such a notion seems outdated in the contemporary era where technological advances have been made and it seems paramount to obtain a scientific and anatomical understanding of the difficulties which a patient faces in therapy. Such a viewpoint is given further credence by the work of Di Leva (2010) who surmises that adopting EBP is essential in an industry (Sports Therapy) which has traditionally been dismissive and unbecoming towards scientific evidence, with the traditional philosophic approach still being part of patient care, but it is being surpassed by the need to incorporate scientific evidence into therapeutic modalities and methods. Manske and Lehecka (2012) also warn about the barriers to integrating EBP into Sports Therapy: therapists may feel that they have a lack of skills or knowledge towards its implementation or else they may not feel confident over the best way in which to implement it. If therapists feel unable to provide the competency which is needed to undertake the rigorous process of EBP, then they may not feel sufficiently qualified to undertake it and perhaps be reluctant to offer it to clients, which could deprive them of the benefits of the treatment.
A further obstacle towards successful EBP is how sports therapists are schooled in it. Olsen et al. (2013) articulate that whilst EBP is a reliable tool in Sports therapy, it can be a difficult concept for students to become educated in as it requires a significant amount of practice to master, often being an ongoing and continuous process, which lasts throughout all of their careers. Olsen et al. (2013) are also mindful of the need to have a strong role model for students to observe how to practice EBP from, something which may come in the form of a mentor or other such figure. Whilst garnering a mentor may be possible, it is also noteworthy that students tend to exhibit a positive attitude towards EBP, even if their skills are deficient in this area (Kim et al., 2009; Glaziou et al., 2008; Lai and Nallilah, 2012). This certainly implies that EBP is worth teaching, particularly if students are positively pre-disposed towards it. How EBP is taught is certainly open to debate, with some favouring a traditional model of teaching (clinical education) and others operating for online and direct teaching methods which have been proven to yield benefits in some students (Schilling et al., 2006; Ilic et al., 2012; Florin et al., 2011). Incidentally, another barrier to successful implementation of EBP is actually searching for and locating the correct information, with Priskil et al. (2009) and Cooper and Elnicki (2011) articulating that some students have difficulties in these areas.
Regardless of the barriers towards EBP, Hoffman et al. (2009) communicate that it is important for health professionals (sports therapists in particular) due to it having the capacity to provide the greatest standard of care possible for patients, as well as allowing them to have access to a more modern style of treatment. Such an argument seems to be given further credence by the fact that Sports Therapy is undeniably a changing and evolving industry, dynamic and diverse and needs an updated approach to complement the intricacies of it. However, it also advisable to note that theory and practice do not align perfectly (Weick, 1979), which calls EBP into question to some degree, although its prevalence and endemic use across multiple disciplines seem to allay any fears about its reliability and feasibility.
Conclusion
In conclusion, EBP is a complex and wide-ranging concept which is multi-faceted. There is a certain sequence of how to carry it out and a process to be followed in respecting its significance. It has become evident over the course of this discussion that EBP is something which is very significant in Sports Therapy, principally because it acknowledges the scientific aspects of the industry, which other approaches do not. It is also important to consider that EBP is something which some students and professionals find hard to learn or grasp, which is evidenced by the fact that numerous studies (as previously mentioned), have illustrated that the research gathering phase of it can be complex. However, with appropriate schooling and instruction, this can be offset. Ultimately, although EBP can be difficult to implement, it contains numerous assets which make it relevant to the Sports Therapy industry.
References
Babbie, E. R. (2010). The Practice of Social Research. 12th edn. Belmont, CA: Wadsworth Cengage.
Cooper, A. L. and Elnicki, D. M. (2011) Resource Utilisation Patterns of Third Year Medical Students. Clin Teach, 8(1):43–47. doi: 10.1111/j.1743-498X.2010.00393.x.
Di Leva, R. (2010). The role of Evidence Based Practice in Sports Therapy. The Journal of Sports Therapy, 3 (3): 6.
Denscombe, M. (2010). The Good Research Guide: For Small-Scale Research Projects. London: Routledge.
Denzin, N.K. (2009). Qualitative inquiry under fire: Toward a new paradigm dialogue. Walnut Creek, CA: Left Coast Press.
Florin, J., Ehrenberg, A., Wallin, L. and Gustavsson, P. (2011) Educational Support for Research Utilization and Capability Beliefs Regarding Evidence- Based Practice Skills: A National Survey of Senior Nursing Students. J Adv Nurs. ; 68(4): 888–897. doi: 10.1111/j.1365-2648.2011.05792.x
Glasziou, P., Burls, A. and Gilbert R. (2008) Evidence Based Medicine and The Medical Curriculum. BMJ, 337. doi: 10.1136/bmj.a1253.
Guyatt, G., Rennie, D., Meade, M. O. and Cook, D. J. (2008). Users’ Guide to Medical Literature: A Manual for Evidence-Based Clinical Practice, 2nd Edition.
Ho, P. M., Peterson, N. P. and Masoudi, A. F. (2008). Evaluating the Evidence: Is there a rigid hierarchy? Circulation, 118: 1675-84. doi: 10.1161/CIRCULATIONAHA.107.721357.
Hoffman, T., Bennett, S. and Del Mar, C. (2009). Evidence-Based Practice Across the Health Professions. Sydney: Elsevier Australia.
Ilic, D., Tepper, K. and Misso, M. (2012) Teaching Evidence Based Medicine Literature Searching Skills to Medical Students During the Clinical Years: A Randomized Control Trial. Journal of the Medical Library Association: JMLA. doi: 10.3163/1536-5050.100.3.009
Kim S. C., Brown, C. E., Fields, W. and Stichler, J. F. (2009). Evidence Based Practice Focused Interactive Teaching Strategy: A controlled study. J Adv Nurs. 65(6): 1218–1227.
Lai N.M. and Nalliah, S. (2012) Information Seeking Practices of An Evidence Based Medicine Training Programme. Educ Heal. 23(1): 151.
Manske, R. C. and Lehecka, B. J. (2012) Evidence Based Medicine/Practice in Sports Therapy. International Journal of Sports Physical Therapy, 7(5), 461–473.
Muijis, D. (2010). Doing Quantitative Research in Education with SPSS. London: SAGE.
Polit, D. F. and Beck, C. T. (2014). Essentials of nursing research: Appraising evidence for nursing practice. 8th edn. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins.
Price, B. (2006). Exploring Person-Centred Care. Nursing Standard, 20 (50): 49-56.
Pruskil, S., Burgwinkel, P., Georg, W., Keil, T. and Kiessling, C. (2009) Medical Students’ Attitudes Towards Science and Involvement in Research Activities: A Comparative Study with Students From a Reformed and Traditional Curriculum. Medical teacher. 31(6): 254–259.
Olsen, N. R., Bradley, P., Lomborg, K. and Nortvedt, M. W. (2013). Evidence Based Practice in Clinical Physiotherapy Education: A Qualitative Interpretive Description. BMC Medical Education, 13, 52. doi:10.1186/1472-6920-13-52.
Rubin, A. and Parrish, D. (2007). Challenges to the Future of Evidence-Based Practice in Social Work Education. Journal of social Work Education, 43, 405-428.
Rubin, A. (2012) Practitioner’s Guide for using Research for Evidence-Based Practice. London: Wiley.
Schön, D. (1991) The Reflective Turn: Case Studies In and On Educational Practice. New York: Teachers Press, Columbia University.
Schilling, K., Wiecha, J., Polineni, D. and Khalil, S. (2006) An interactive Web-Based Curriculum on Evidence Based Medicine: Design and Effectiveness. Fam Med; 38(2): 126–132.
Strauss, S. E. [et al.] (2005). Evidence Based Medicine: How to Practice and Teach. Edinburgh; New York: Elsevier/Churchill Livingstone.
US Department of Health and Human Services (2015). Glossary of Terms. [Online]. Available at: http://effectivehealthcare.ahrq.gov/index.cfm/glossary-of-terms/?pageaction=showterm&termid=24 (Accessed: 12 March 2015).
Weick, K.E. (1979). The social psychology of organizing. 2nd edn. Reading, MA: Addison-Wesley.
World Health Organisation (2010). Framework for Action on Interprofessional Health Education. [Online]. Available at: http://www.who.int/hrh/resources/framework_action/en/ (Accessed: 12 March 2015).